Heavy Bleeding (Menorrhagia)
Uterine causes
In some instances, the cause of heavy vaginal bleeding will remain unknown but most causes of abnormal or heavy bleeding can be identified. These can be broadly separated into
- Hormonal or Non-Structural
- Structural (Fibroids, adenomyosis, polyps, cancer, etc).
Specific causes include
- Hormonal conditions This may arise from obesity, insulin resistance, thyroid problems or polycystic ovary syndrome (PCOS)
- Anovulation – This is a dysfunction of the ovaries, namely when a woman fails to ovulate (i.e. her ovaries don’t release an egg) during her period. This means that her body doesn’t produce the progesterone hormone as it normally would during the menstrual cycle. This is typical among adolescent girls in the first year of ovulation;
- Fibroids common benign (non-cancerous) tumours.
- Adenomyosis
- Endometrial polyps
- Cesarean section scars
- IUDs a common side effect of using a non-hormonal intrauterine device for birth control;
- Medications – medicine for anti-inflammatory complaints, hormonal issues (e.g. oestrogen and progestin) as well as anticoagulants;
- Endometrial hyerplasia, endometrial carcinoma, and cervical carcinoma
- Pregnancy Complications – A single, heavy, late period may be due to a miscarriage. Also, retained placental tissue can cause bleeding many months after delivery
- Inherited Bleeding Disorders – for example, Von Willebrand disease. This is a condition where an important blood-clotting regulator is deficient or impaired
Hormonal Causes oF Abnormal Uterine Bleeding
Hormonal Imbalance
Hormonal imbalance - too much, or too little- can affect the endometrium and cause abnormal bleeding. Any condition that affects the endometrium can naturally cause abnormal bleeding.
Low progesterone or unopposed estrogen
If your doctor says your heavy periods are the result of “hormone imbalance,” it may mean you’re having anovulatory cycles and are not making the progesterone you need to thin the uterine lining and prevent heavy periods. In other words, you have estrogen that is “unopposed” by progesterone and so develop a thickened uterine lining.
The only way to make progesterone is to ovulate, so, if you don’t have progesterone, it’s because you’re not ovulating. The next question is “why are you not ovulating?” Here are some possibilities.
- You have PCOS, in which case, your best treatment is to reverse PCOS so you can ovulate and make progesterone and prevent heavy periods.
- You have thyroid disease or high prolactin.
- You’re a teenager so too young to ovulate regularly. It’s a temporary situation that you will probably outgrow. In the meantime, you can lighten your flow with a dairy-free diet, turmeric, and iron (see below).
- You’re in perimenopause or which is when ovulation starts to wind down and you lose progesterone. This type of heavy bleeding is also called dysfunctional uterine bleeding
Your doctor might not be able to figure out if you’re ovulating or if you have enough progesterone. You can test yourself by tracking your basal body temperatures.
Thyroid disease
is a common and treatable cause of heavy menstrual bleeding. Experts say that thyroid function should be evaluated in all cases of heavy menstrual bleeding and doing so “would avoid unnecessary surgeries and exposure to hormones.” Women are twenty times more likely to have a thyroid issue than men. As a major hormone-producing gland, an over or underactive thyroid can be detrimental to one’s health. There are various thyroid diseases and conditions, including Hashimoto’s Disease, where the immune system confuses the thyroid for a foreign structure and attacks it, thinking it’s defending the body.
Ask your doctor to test your thyroid and then ask to see the results. If your TSH is higher than 3 mIU/L, it could be a sign of subclinical hypothyroidism (underactive thyroid).Also, if you have thyroid disease in your family, look at the test “thyroid antibodies” or “TPO antibodies,” which is the marker of autoimmune thyroid disease or Hashimoto’s disease. Autoimmune thyroid disease affects one in four women and can cause symptoms of underactive thyroid (including heavy periods) even when TSH is normal.
Hormonal Causes of Bleeding
Atrophy- Too thin
Atrophy- Too thin
Atrophy- Too thin

When the endometrium becomes too thin, it becomes friable and more easily bleeds. Atrophy is the most common cause of bleeding among post menopausal patients. It may also occur in some premenopausal patients on long term hormonal contraceptive use (oral contraceptive pills) due to prolonged suppression of the endometrium.
Ovarian Atrophy
Atrophy- Too thin
Atrophy- Too thin

Ovarian atrophy starts to develop during the perimenopausal period, and is normal in postmenopausal patients. The lack of hormonal support then leads to thinning of the endometrium. This can result in abnormal uterine bleeding among postmenopausal patients, but is not associated with pain.
Small inactive ovaries may also be seen in women with premature menopause, or some women on long term oral contraceptive pills due to prolonged suppression.
Cystic Hyperplasia- Too thick
Cystic Hyperplasia- Too thick
Cystic Hyperplasia- Too thick

Hyperplasia may be seen with excessive unopposed estrogen, tamoxifen and in some patients with polycystic ovarian syndrome. Endometrial hyperplasia is usually caused by an excess of estrogen without progesterone (female hormones). The lining of the uterus is not shed if ovulation does not occur. This means that the endometrium may continue to grow in response to the production of estrogen. The cells of the endometrium may abnormally crowd (hyperplasia), which may lead to the cancer of the uterus.
Atypical endometrial hyperplasia is a premalignant condition of the endometrium. It occurs when there is an overgrowth of abnormal cells, or it may develop from endometrial hyperplasia. In some cases, polyps (tumors) in the uterus can lead to atypical endometrial hyperplasia. It is caused by unopposed estrogen from a number of factors including:
- Hormone changes during menopause (cessation of menstrual period)
- Polycystic ovarian syndrome
- Estrogen-hormone replacement therapy
- Breast cancer treatment, using drugs such as tamoxifen (Nolvadex®, Tamofen®)
Polycystic Ovarian Syndrome
Cystic Hyperplasia- Too thick
Cystic Hyperplasia- Too thick

Polycystic ovarian syndrome (PCOS) is a common hormonal condition, affecting about 15% of patients of reproductive age. Hormonal imbalance includes high levels of Luteinizing hormone (LH), which leads to anovulation, and may lead to high levels of insulin and testosterone, Patients may have hirsuitism (excess hair growth) and acne. This increases the risk of type 2 diabetes and other conditions.
Hormonal imbalance can result in irregular periods, few periods (oligomenorrhea) or no periods (amenorrhea). The ultrasound appearance is characterized by multiple small follicles. In about half of cases, the ovaries are also enlarged in size.
Structural (Non Hormonal) Causes of Bleeding
Fibroids
Endometrial Polyps
Adenomyosis

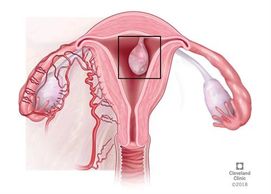
Fibroids are benign (non cancerous) growths or tumors of the uterine wall. The uterine wall is primarily smooth muscle, and fibroids are tumors of the muscle tissue. They are common, especially over the age of 30, but can also affect younger women. They tend to run in families (if your mother or sister have fibroids, then you are more likely to have them also). Most women with fibroids are not aware of them because they don't cause symptoms. However, they are a common cause of bleeding- especially those closer to the lining of the uterus (endometrium). They can also cause cramping bit they don't usually cause severe pain.
Adenomyosis
Endometrial Polyps
Adenomyosis

Adenomyosis is usually a more diffuse process involving the uterus, unlike the discrete growths of fibroids. Adenomyosis may be considered as the cells which compose the endometrium or lining into the wall of the uterus. This may cause both bleeding and pain with your cycle
Endometrial Polyps
Endometrial Polyps
Cesarean section scar
Polyps are benign growths of the lining, or endometrium, similar to fibroids being benign growth of the wall of the uterus. These are relatively common, but not as common as fibroids. They may cause intermenstrual bleeding (between periods). They can be easily overlooked unless specifically sought because they blend in with the normal endometrium
Cesarean section scar
Endometrial hyperplasia, cancer
Cesarean section scar

Cesarean section scars from prior cesarean deliveries is a much more common cause of pain and bleeding than patients, and physicians, realize. Unfortunately, our bodies have a memory. The scar produced from the cesarean incision never goes away completely. Symptoms of pain and/ or bleeding seem to be more common when the scar is bigger- when it doesn't close completely, or perhaps reopens. Women with multiple cesarean deliveries have a higher chance of pain. This can produce scarring along the uterine-bladder interface, and alterations in the appearance of the uterus. In addition to the scar itself as a source of pain, in some patients endometriosis (growth of endometrial cells) may affect the cesarean scar.
IUD
Endometrial hyperplasia, cancer
Endometrial hyperplasia, cancer

IUDs can irritate the endometrium, especially if not correctly positioned. Malpositioned IUDs are common
Endometrial hyperplasia, cancer
Endometrial hyperplasia, cancer
Endometrial hyperplasia, cancer
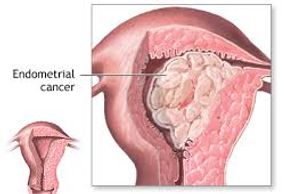
Hyperplasia represents benign over growth of the endometrium. Endometrial cancer is uncontrolled growth of endometrial cells. When women speak of uterine cancer, it is usually cancer of the cervix, or endometrium.
Endometrial cancer most often presents with postmenopausal bleeding, but about 15% of cases affect premenopausal women and 4% affect women 40 or younger.
Common Ultrasound appearances of uterine bleeding

Fibroids
Fibroids appear as discrete structures in the wall of the uterus, although sometimes they grow into the uterine cavity. Fibroids closest to the uterine cavity (endometrium) are most likely to cause symptoms of bleeding.
Types of Fibroids
- Intramural fibroids – They develop in the muscle of the womb.
If large enough, they can distort the shape of the uterus and cause heavy periods, pain and pressure. - Subserosal fibroids – they originate in the muscle wall but protrude outside the womb into the pelvis.
- Submucosal fibroids – they grow into the inner cavity of the womb and are more likely to cause bleeding problems or difficulties when trying to conceive.
In almost all cases, the fibroids will shrink and may eventually disappear after menopause.

Adenomyosis
Adenomyosis typically presents with an enlarged uterus. The myometrium is thickened and non-uniform (heterogeneous) with a 'streaky' appearance. Fibroids are often absent, but co-existing fibroids are not unusual.

Polyps
Adenomyosis typically presents with an enlarged uterus. The myometrium is
Endometrial polyps show as focal echogenic areas which obscure the normal central interface. A vascular pedicle, when present, helps to confirm a polyp.
Cervical Cancer
Cervical Cancer

Cervical cancer is an uncommon but important potential cause of bleeding. However, like other cancers, early stages are usually not symptomatic. Women should have regular checkups and cervical swabs. We mention it here, but actually is a uterine cause.
Almost all cervical cancer cases occur in women who have been previously infected with HPV. There are more than 100 different types. As most types of HPV do not cause any symptoms, you or your partner could have the virus for months or years without knowing it. At least 15 types of HPV are considered high-risk for cervical cancer. The 2 highest risk are HPV 16 and HPV 18, which cause the majority of cervical cancers.
HPV is spread during sexual intercourse and other types of sexual activity, such as skin-to-skin contact of the genital areas or using sex toys, and is very common. Most women will get some type of HPV infection at some point in their lives. Some types of HPV do not cause any noticeable symptoms and the infection will pass without treatment.
Others can cause genital warts although these types are not linked to an increased risk of cervical cancer.
High-risk types of HPV are thought to stop the cells working normally, which can eventually cause them to reproduce uncontrollably, leading to the growth of a cancerous tumour.
Abnormal Bleeding
A video of abnormal bleeding, including fibroids, from the Mayo Clinic
BGCS Endometrial Guidelines 2017 (pdf)
DownloadMenorrhagia (pdf)
DownloadVitamin D and fibroids (pdf)
DownloadTransvaginal ultrasound for endometrial cancer (pdf)
DownloadImaging of the Endometrium (pdf)
DownloadUPA treatment of fibroids (pdf)
Downloadwhat-every-woman-should-know-about-cervical-cancer-and-the-human-papilloma-virus-handout (pdf)
Download