HORMONES, and HORMONE REPLACEMENT THERAPY
HORMONES AND Normal Menstrual Cycle

Alterations During Your Menstrual Cycle
Even when you're not pregnant or don't want to be, your body is programmed to be a potential incubator. In order to achieve this, your brain and ovaries are constantly changing hormone level during each monthly cycle.
Your reproductive system is under the influence of hormones regulated by the hypothalamus and its gonadotropin-releasing hormone (GnRH). This hormone causes the cells in the frontal part of the pituitary gland to produce two types of hormones.
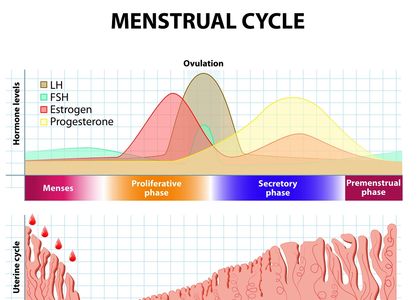
The first is the FSH or follicle-stimulating hormone, and the other is LH, or luteinizing hormone. These hormones travel all the way to the ovaries where they influence estrogen and progesterone level changes and aid maturing of the follicles inside the ovaries. This complex hormone interaction is called hypothalamic-pituitary-ovarian axis.
At the end of the previous cycle, the gonadotropin-releasing hormone levels increase due to negative feedback of estrogen and progesterone (their levels drop right before periods), which also causes the increase of the follicle stimulating hormone levels.
All the hormones involved in hypothalamic-pituitary-ovarian axis rise in one period of menstrual cycle and drop in the other. All of these fluctuations have to do with ovulation, and can cause symptoms like acne, bad mood, or appetite changes.
The Corpus Luetum
The Corpus Luetum
LH and FSH stimulate a dominant follicle to grow and develop. In the last stages, the cells surrounding the egg will produce estradiol. A surge in LH production by the anterior pituitary gland normally occurs at approximately day 14 of the menstrual cycle. This stimulates the release of the egg from the ovulatory follicle which then becomes the corpus luteum. The corpus luteum releases progesterone, which prepares the body for pregnancy. If the egg is not fertilised, the corpus luteum breaks down and the production of progesterone drops. The drop in progesterone, in turn, causes the endometrium to break down with onset of menstrual bleeding, marking the start of a new menstrual cycle.
if the ovulated egg is fertilised, the cells that surround the early embryo (which are destined to form the placenta) will secrete human chorionic gonadotropin (HCG). This hormone has a similar chemical structure to LH and so helps to support the corpus luteum which then continues to produce progesterone until the placenta is established.
If progesterone is absent or levels are too low, irregular and heavy menstrual bleeding can occur. Lack of progesterone can mean the ovary has failed to release an egg at ovulation, as can occur in women with polycystic ovarian syndrome (PCOS).
A drop in progesterone during pregnancy can result in a miscarriage and early labour. Mothers at risk of giving birth too soon can be given a synthetic form of progesterone to delay the onset of labour. Vaginal progesterone is also given to women at risk of preterm birth to strengthen the cervix.

Normal Menstrual Cycle: Ovaries seen by ultrasound

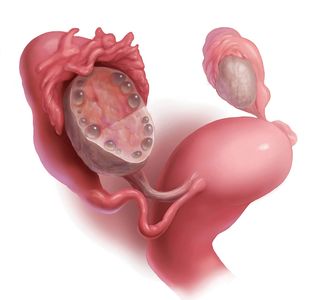
Follicular phase
During the follicular phase of the cycle, multiple follicles develop with increasing estrogen levels.
Estrogen has a lot to do with other aspects of women's health, like mood stability, protecting bone health, keeping cholesterol levels under control and appearance of the skin.

Ovulation
A dominant follicle develops which releases an egg. This means the covering of the ovary has to rupture to release the egg. This can sometimes cause bleeding of adjacent blood vessels and produce significant pain and a hemorrhagic (blood containing) cyst.
The cervical mucus increases in quantity and becomes clear and more elastic at this phase.

Luteal Phase
Common symptoms of the luteal phase include all of the known symptoms of the premenstrual phase, such as:
- Increased appetite
- Tiredness
- Breakouts
- Fatigue due to premenstrual syndrome
- Oily hair and skin.
In the late luteal phase, hormone levels (progesterone and estrogen) start to decrease if there is no conception. Some of the common menstrual symptoms include cramping, tenderness of the skin and breasts, mood swings, tiredness, headaches and migraines. The average duration of menstruation is from 4 to 6 days. But if your periods last for 2-8 days it is considered to be normal.

Steroid Metabolism showing Progesterone and Estrogens
Sex HOrmones
Estrogen (Oestrogen)
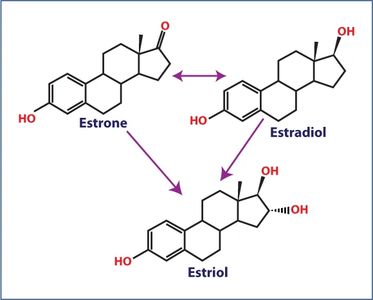
Estrogens (Oestrogens) are steroid hormones present in both men and women, but present at significantly higher levels in women of reproductive age. There are three naturally occurring estrogens in women: estrone (E1), estradioil (E2), and estriol (E3). It's worthwhile reviewing steroid metabolism. Pregnenolone is formed from cholesterol (Vitamin D is also form from cholesterol!) Progesterone can be metabolized to any of the estrogens, as well as cortisol.
The developing follicles in the ovaries are responsible for producing the majority of the estrogens. There is also evidence that some estrogens are formed by the liver, adrenal glands, muscle tissue, fat cells and possibly the brain. Synthesis of estrogens occurs in the theca interna cells of the developing ova, and is accomplished through conversion of androstenedione, either from progesterone or an alternative route, from cholesterol. E2 can be converted to E1 and E3. E1 can be converted to E2 or E3. However, E3 is not interconvertible and so importantly, does not result in an increase of either of the other two estrogens
Estradiol (Oestradiol) is strongest of the three naturally produced estrogens. It has many functions, although it mainly acts to mature and maintain the female reproductive system. A natural increase in blood estradiol concentrations during the menstural cycle causes an egg to mature and be released; that is, to be ovulated. Another important role of estradiol is to thicken the lining of the uterus so that the egg can implant if it becomes fertilised. Estradiol also promotes development of breast tissue and increases both bone and cartilage density.
Estradiol levels vary throughout the monthly menstrual cycle, being highest at ovulation and lowest at menstruation. Estradiol levels in women reduce slowly with age, with a large decrease occurring at menopause when the ovaries ‘switch off’. In pregnant women, the placenta also produces a lot of estradiol especially towards the end of the pregnancy.
Men also produce oestradiol; however, the amounts produced are much lower than in women. Within the testes, some testosterone is changed into oestradiol and this estradiol is essential for the production of sperm. In both sexes, estradiol is also made in much smaller amounts by fat tissue, the brain and the walls of blood vessels.
Estriol
Oestriol (Estriol) is one of three oestrogens (estrogens) naturally produced by women. Normally, levels in the body are very low, but during pregnancy, it is made in much higher amounts by the placenta. Oestriol levels increase throughout pregnancy and are highest just before birth. It is an indicator of the health of the unborn fetus because the chemical from which it is made in the placenta, comes from another chemical which is first made in the baby’s adrenal glands and then gets altered in the liver of the baby before being finally converted to oestriol in the placenta. It causes growth of the uterus and increases its sensitivity to other pregnancy-related hormones, thus causing a gradual preparation for birth. Oestriol levels start to increase from week eight of pregnancy and scientists now think that labour begins when oestriol becomes the dominant hormone.
How is oestriol controlled?
Oestriol is made by the placenta from a chemical that comes from the fetus. The fetal adrenal glands first make a hormone called dehydroepiandrosterone sulphate (DHEAS). DHEAS is then transported to the fetal liver and made into 16a-hydroxy-DHEAS. The 16a-hydroxy-DHEAS is in turn transported to the placenta where it is then made into oestriol. For most of pregnancy, most of the oestriol made is bound to other chemicals thereby preventing the oestriol from exerting any biological effects.
What happens if I have too much oestriol?
A sudden surge in oestriol happens around three weeks before labour. If the surge comes early, this can suggest a premature birth. Some hormone replacement therapy (HRT) preparations contain oestriol. Although the body removes oestriol much faster than other oestrogens, there are positives and negatives to its use in HRT.
What happens if I have too little oestriol?
In non-pregnant women, oestriol only exists at very low levels. Too little unbound oestriol during pregnancy can indicate that there are problems with the baby, such as Down’s syndrome, or problems with the placenta. Later in pregnancy, comparatively low oestriol indicates that labour may not come on its own, but will have to be induced.
Some of the most common and effective treatments that employ estriol include: hot flashes, insomnia, skin enhancement, vaginal atrophy and reduced frequency of urinary tract infections. Most recently, estriol has shown the potential to treat individuals with Th1-mediated autoimmune illnesses, including multiple sclerosis and rheumatoid arthritis.
Progesterone
Progesterone is a hormone that controls menstruation and fertility. It is produced by the female body in the second half of the menstrual cycle, after ovulation (yellow in chart). Progesterone gets the endometrium ready for pregnancy post ovulation.
Adequate progesterone levels are very important for a woman’s health. Hormonal imbalances due to low progesterone can cause serious harm to both pregnant and non-pregnant women. Moreover, progesterone allows the embryo to survive and gives immunity to the developing baby.

Site Content
Low progesterone levels / Estrogen dominance may cause the following problems:
- Miscarriage
- Infertility
- Uterine bleeding
- Vaginal dryness
- Hair thinning
- Fatigue, loss of sleep
- Decreased sex drive
- Weight gain
- Mood swings
- Anxiety or depression
- Headaches or migraines
- Breast, endometrial cancers.
How to increase progesterone
1. Progesterone is synthesized from pregnenolone, which in turn is synthesized from cholesterol. So to ensure high progesterone levels, it is important to change your diet to include foods that give you adequate cholesterol.
2. Turmeric can be very useful in boosting progesterone production. Consuming curries with high turmeric content can be very good for your body’s progesterone levels. Other herbs like thyme and oregano also have the same properties.
3. Vitex (Vitex agnus-castus) is a plant used in herbal medicine. Vitex may influence hormone levels in a number of ways. For example, it's said to promote the release of luteinizing hormone and, in turn, increase levels of progesterone. Vitex is also thought to affect levels of prolactin, which is involved in stimulating breast development and milk production in women.
4. Eat more foods that are rich in vitamin B, more specifically vitamin B6.
5. Follow a diet that is low in conventional meat products as the hormones given to the animals often act as estrogen in the body, reducing progesterone levels. It is best to try organic and grass-fed produce.
6. Make sure there’s enough magnesium in your diet with foods like black beans, spinach, halibut, whole grain cereals, and nuts
7. Zinc is one of the most important minerals which balances the hormones at the right levels. It also plays an important role in fertility as it prompts the pituitary gland to secrete follicle-stimulating hormones, which promotes ovulation in the female body. Foods like liver, red meat, shellfish, dark chocolate consist of high amounts of zinc in them.
8. Avoid xenoestrogens that wreak havoc on your hormones. Xenoestrogens cause our body to believe that estrogen levels are high and progesterone levels suffer as a consequence. These are found in plastics, synthetic hormones and animal products. Avoiding them can boost progesterone levels in your body.
9. Enhance your protein intake. Protein is essential for any hormone production.
10. Consume food high in micro-nutrients like vegetable, fruits and leafy greens. Micro-nutrients boost progesterone production.
11. Bio-identical progesterone cream can be used as a supplement for low progesterone. However, make sure you read the ingredients of the cream before you start using them. Some creams have high estrogen content along with the natural progesterone so using those will not be helpful to your cause.
12. Destress. When adrenal glands are exhausted due to stress, the body produces cortisol instead of progesterone.
13. Vitamin E helps increase the luteal blood flow which lengthens the luteal phase, i.e. the egg released will be if higher quality increases the chances of pregnancy in women. Therefore, vitamin E plays an important role in pregnancy. Foods like nuts, sunflower seeds, and olive oil are rich in vitamin E and should be consumed in order to be fertile.
Too Much or Too Little Estradiol
High or Low Levels of Estradiol
What happens if I have too little estradiol?
In women, too much estradiol can have a number of effects. In mild cases, excess oestradiol may cause acne, constipation, loss of libidoand depression. More severe effects can include, weight gain infertility, stroke, heart attack and an increased risk of developing uterine and/or breast cancer.
In men, too much estradiol can also cause sexual dysfunction, loss of muscle tone, increased body fat and the development of female characteristics, such as breast tissue. Estradiol becomes more dominant as a man ages and his testosterone production reduces, which scientists think may be a contributing factor in the development of prostate cancer.
The combined oral contraceptive pill (the pill) contains synthetic forms of both progesterone and oestradiol. The pill works by preventing ovulation, making it nearly 100% effective in preventing pregnancy. As well as preventing ovulation, the synthetic hormones make the cervical mucus thicker and therefore more difficult for the sperm to move through, thereby reducing their chances of getting to the uterus and oviducts. The synthetic estradiol was added to prevent breakthrough bleeding, which sometimes occurs with the progesterone-only pill (the mini pill).
What happens if I have too little estradiol?
Estradiol is necessary for bone development, so people with low oestradiol tend to have skeletal problems like inadequate bone growth and osteoporosis. Girls will also encounter problems at puberty such as a delay in, or failure of, breast development, a disrupted or absent menstrual cycle and infertility. Estradiol also has important roles in the brain, where low levels can cause depression, fatigue and mood swings.
A woman’s estradiol production falls naturally at the menopause and causes many of its symptoms. Initially these include night sweats, hot flushes, vaginal dryness and mood swings, while in the long term she is more likely to develop osteoporosis. Estradiol is used in hormone replacement therapy to relieve these symptoms of the menopause in women.
Polycystic Ovarian Syndrome
Polycystic Ovarian Syndrome (PCOS)
Polycystic ovarian syndrome (PCOS) may cause irregular menses and contribute to infertility. In clinical practice, 75% of women with PCOS suffer from anovulation infertility and 50% of them experience recurrent pregnancy loss.
Additionally, the chronic anovulation seen in PCOS implies prolonged estrogen excess or lack of progesterone and results in atypical endometrial hyperplasia, which is the precursor of endometrial carcinoma
Patients with PCOS also have a much higher chance of developing dermoid tumors.
Also, see blog post

Ultrasound
Diagnosis
PCOS is a “syndrome,” or group of symptoms that affects the ovaries and ovulation. There is no single test to definitively diagnose PCOS. However, the Rotterdam criteria are generally accepted with the diagnosis of polycystic ovary syndrome (PCOS) made in the presence of 2 of the following 3 conditions:
- oligo-ovulation or anovulation, usually seen as irregular or skipped perioids.
- high levels of male hormones manifested by the presence of either hirsutism or elevated hormone levels (including serum testosterone androstenedione and/or dehydroepiandrosterone sulfate)
- ultrasound finding of multifollicular ovaries (≥12 follicles with a diameter of 2 mm to 9 mm in one or both ovaries; or ovarian stromal volume of 10 mL or more. The small ovarian follicles are typically peripheral in location. This may be described as polycystic ovarian morphology (PCOM), which may occur without the other conditions. Realize that PCOM does not necessarily mean PCOS, and there are other causes of the ultrasound appearance, including hypothalamic amenorrhea (more below).
The cause of PCOS remains unknown. However, we know that many women with this condition have decreased sensitivity to insulin, called 'insulin resistance.' Insulin, a hormone produced by the pancreas, is necessary to carry sugar from the bloodstream into the cells, where it is converted into energy. When cells are resistant to insulin, it means that the effect of insulin on sugar, and other functions, is deficient. More insulin than normal is required to be produced by the pancreas to ensure that the body cells absorb enough sugar. This leads to high insulin levels in the blood stream which, among other effects, make the ovaries overproduce male hormones, leading to a hormone imbalance that triggers or worsens some of the symptoms of PCOS. Eventually, the pancreas may not be able to maintain the high insulin levels necessary to keep sugar levels normal and the patient develops diabetes.

TREATMENT
Diet and Lifestyle
There is no known cure for PCOS, just as there is no single method to diagnose it. However, diet, exercise and medical treatment can greatly help. Die and lifestyle interventions are among the first-line treatments for PCOS. Losing just 5 to 10 percent of your body weight can help regulate your menstrual cycle and improve PCOS symptoms. Weight loss can also improve cholesterol levels, lower insulin, and reduce heart disease and diabetes risks. Weight reduction through energy restriction has been shown to exert positive influences on both metabolic and hormonal aspects of this condition. Although it is likely that diet is not the root cause of PCOS, it represents a modifiable variable with the potential to improve the health of women with this condition. Any diet that helps you lose weight can help your condition. However, some diets may have advantages over others. Studies comparing diets for PCOS have found that low-carbohydrate diets are effective for both weight loss and lowering insulin levels. A low glycemic index diet that gets most carbohydrates from fruits, vegetables, and whole grains helps regulate the menstrual cycle better than a regular weight loss diet.
Exercise also has positive effects. A few studies have found that 30 minutes of moderate-intensity exercise at least three days a week can help women with PCOS lose weight. Losing weight with exercise also improves ovulation and insulin levels. Exercise is even more beneficial when combined with a healthy diet. Diet plus exercise helps you lose more weight than either intervention alone, and it lowers your risks for diabetes and heart disease.
If you have been having irregular periods and some of the other symptoms of polycystic ovary syndrome, please see your GP, gynecologist or an endocrinologist. Early treatment of PCOS can contribute to your long-term health, and improve your quality of life. Staying as healthy as possible is the goal. Try to stay on a healthy diet with adequate amounts of protein, as well as whole grains and lots of fruits and vegetables. Exercise regularly to keep your weight in check, improve your body's response to extra insulin, and reduce your risk of diabetes, heart disease, and stroke. Exercise for 30 minutes 3-5 times a week is very beneficial. Because of the possible increased risk of cardiovascular disease, women with PCOS should also have their blood pressure checked regularly. You should also monitor your levels of bad cholesterol (LDL), good cholesterol (HDL), and triglyceride levels.With proper diagnosis and treatment, most PCOS symptoms can be reversed or at managed and your risk of complications greatly minimized.
ORAL CONTRACEPTIVE PILLS (OCP)/ BIRTH CONTROL PILLS
Birth Control Pills
Oral contraceptive pills (OCP) work to suppress both the ovaries and the endometrium. All OCPs contain a small amount of man-made estrogen and progestin hormones. These hormones work to inhibit the body's natural cyclical hormones to prevent pregnancy. Pregnancy is prevented by a combination of factors:
- It suppresses the ovary and prevents release of an egg each month
- thickens the mucus in the neck of the womb, so it is harder for sperm to penetrate the womb and reach an egg
- thins the lining of the womb, so there is less chance of a fertilised egg implanting into the womb and being able to grow. In fact, suppression of the endometrium may be even more effective than suppression of the ovaries.
The pill is over 99% effective if used correctly. Some women find it difficult to take the pill at the same time every day, and it's less effective if not used correctly. Other methods of contraception are better at preventing pregnancy, such as the IUD, IUS, implant and injection. OCPs are not recommended, for women over age 35 who smoke. If you don't smoke, you can use hormonal contraceptives until menopause. There are many different brands of pill, with three main types offered through the NHS:
Monophasic 21-day pills
This is the most common type. Each pill has the same amount of hormone in it. One pill is taken each day for 21 days and then no pills are taken for the next seven days. Microgynon, Marvelon, Yasmine and Cilest are examples of this type of pill.
Phasic 21-day pills
Phasic pills contain two or three sections of different coloured pills in a pack. Each section contains a different amount of hormones. One pill is taken each day for 21 days and then no pills are taken for the next seven days. Phasic pills need to be taken in the right order. Logynon is an example of this type of pill.
Every day (ED) pills
There are 21 active pills and seven inactive (dummy) pills in a pack. The two types of pill look different. One pill is taken each day for 28 days with no break between packets of pills. Every day pills need to be taken in the right order. Microgynon ED is an example of this type of pill.Follow the instructions that come with your packet. If you have any questions, ask your GP, practice nurse or pharmacist.It's important to take the pills as instructed, because missing pills or taking them at the same time as certain medicines may make them less effective.
Another option (not available in the NHS) for hormonal contraceptives is the extended-cycle pill, such as Seasonale. It contains the same hormones as other OCPs but the hormones are taken in a longer cycle. That reduces the number of menstrual periods from 13 periods a year to only four a year.

CONTRACEPTION HORMONAL IUDS or IUS
Hormonal IUDs
The hormonal IUD has also been termed an intrauterine system, or IUS. It is different from other types of hormonal birth control in that it does permit some ovulation and natural cycling. Other good things about the hormonal IUD are that it dramatically decreases menstrual flow and can give some relief for endometriosis. It is most commonly a T shaped plastic device that's put into your womb (uterus) by a doctor or nurse.
It releases the hormone progestogen to stop you getting pregnant and lasts for 3 to 5 years.
Two brands of IUS are used in the UK: Mirena and Jaydess.
Pros
- Unlike all other types of hormonal birth control, Mirena does not completely shut down ovulation and hormone production. Officially it doesn’t suppress ovulation at all, bu it does suppress ovulation in 85 percent of cycles during the first year (when the dose of the levonorgestrel drug is higher), and then in 15 percent of cycles after that. Remember, ovulation is beneficial because it’s the only way to make estradiol and progesterone.
- Compared to pills and implants, the IUS delivers a lower dose of the drug. The blood level of levonorgestrel in Mirena users is about one-tenth that of Pill users. But even that low dose can cause mood and other side effects (see below).
- It’s more effective than almost any other method, with a success rate of over 99%.
- After insertion, you don’t need to do anything or take anything, and it lasts three years (Skyla) or 5 years (Mirena).
- Officially, fertility returns to normal almost as soon as you remove it.
- It reduces menstrual flow by at least 90%, and that’s a huge Pro for very heavy menstrual bleeding.
- It can relieve some of the symptoms of endometriosis.
Cons:
- The hormonal IUD releases the contraceptive drug levonorgestrel, which is not progesterone. The systemic effects of levonorgestrel include acne, hair loss, hirsuitism, depression, anxiety, headaches, breast pain, yeast infections and weight gain.
- It causes ovarian cysts in 5% of users.
- It damages the vaginal microbiome and increases the risk of yeast infections and bacterial vaginosis.
- It suppresses ovulation some of the time. (Not all the time like the pill, implant, injection, or Nuvaring.)
- It can cause irregular bleeding and spotting during the first three to six months of use. After that, it may completely suppress bleeding or permit a light period. (And in case you’re wondering—yes, that light period is the result of a real menstrual that includes ovulation and the making of progesterone.)
- Insertion could be painful. But just to clarify: It’s an in-office procedure that takes a few minutes—it’s not surgery.
- It could come out. The chance of expulsion is about 5 percent, but it’s more common in younger women, breastfeeding women, and in women who had it inserted immediately following childbirth.

IUD
Video on IUD
CONTRACEPTION HORMONAL IUDS or IUS- Complications
Hormonal IUDs- Complications
The most common complication is malposition or perforation on insertion. This is why some prefer ultrasound monitoring of IUD insertion, or ultrasound confirmation of correct placement
Cons:
- The hormonal IUD releases the contraceptive drug levonorgestrel, which is not progesterone. The systemic effects of levonorgestrel include acne, hair loss, hirsuitism, depression, anxiety, headaches, breast pain, yeast infections and weight gain.
- It causes ovarian cysts in 5% of users.
- It damages the vaginal microbiome and increases the risk of yeast infections and bacterial vaginosis.
- It suppresses ovulation some of the time. (Not all the time like the pill, implant, injection, or Nuvaring.)
- It can cause irregular bleeding and spotting during the first three to six months of use. After that, it may completely suppress bleeding or permit a light period. (And in case you’re wondering—yes, that light period is the result of a real menstrual that includes ovulation and the making of progesterone.)
- Insertion could be painful. But just to clarify: It’s an in-office procedure that takes a few minutes—it’s not surgery.
- It could come out. The chance of expulsion is about 5 percent, but it’s more common in younger women, breastfeeding women, and in women who had it inserted immediately following childbirth.

Symptoms of Hormonal Imbalance

Symptoms of a Hormone Imbalance
Hormone production increases during puberty and reaches a peak in healthy adults during their 20s and early 30s. Whether we like it or not, hormone levels then start to decline beginning around our mid-30s to early 40s and continue to remain at lower levels for the remainder of our lives. This decline in hormone levels can cause a variety of symptoms that affect overall quality of life but we can still help control how rapidly or smoothly this change happens and how we adapt to its effects.
Menopause is defined as 12 months after the last menstrual period. The average age for menopause for women in the United States is 51, but some women can start menopause as early as 30. If the onset of menopause happens before the age of 40, it is referred to as premature menopause.
Menopause does not happen suddenly over night. Instead, the drop in hormones is gradual over a period of years. It is common to feel the effect of falling hormones before menopause. This typically begins around the age of 35 for women and 50 for men, but can occur earlier due to toxins in our environment that disrupt our bodies. Your cycle can vary a great deal as your ovaries start to 'sputter', so that you may experience more irregularity in your cycle. This 'sputtering' helps explain the higher chance of twins with aging.
Over time, menopause can also cause other health problems, such as osteoporosis, which is the weakening of the bones.
We can determine your hormonal status with both ultrasound and blood tests.
Even before menopause, your ovaries will gradually become smaller and show fewer and smaller follicles on ultrasound exams.
Blood tests can exclude other conditions such thyroid disease and can measure your estrogen and hormone levels. An estrogen level of 30 or less may indicate you are in menopause. A high level of follicle stimulating hormone (FSH), typically over 40, also indicates that your ovaries are producing less estrogen and typically signals menopause.
Because the symptoms that accompany hormonal imbalance are common to other conditions, they often are misdiagnosed. Symptoms of hormonal imbalance include:
- Irregular periods
- fatigue
- difficulty sleeping
- reduced mental focus (brain fog)
- weight gain
- Hot flashes
- Mood swings
- Decreased cognitive function
- Decreased bone density
- Decreased sex drive
- Night sweats
- Changes in feminine health
- Sleeping issues
- And more
But hormone depletion is not limited to these symptoms. Decreased estrogen, progesterone and testosterone, if left untreated, can lead to chronic health problems.
BIOIDENTICAL Hormonal replacement therapy

Hormone Replacement Therapy (HRPT) for Women.....and Men
Hormones help control and regulate growth and development, tissue function, digestion, excretion, metabolism, respiration, sensory perception, stress, mood, sleep, reproduction, and lactation. Many hormones operate by cascades, where one hormones actives another until the biochemical process that the chain of hormones is intended for is complete.
With 50 different hormones triggering distinct events throughout the body, distinguishing which hormones may be causing health problems becomes complicated. Since these biochemical events can be complex and, at times, interwoven, it’s beneficial to understand your body’s unique tendencies and how they can impact your overall health.
Women are twenty times more likely to have a thyroid issue than men. As a major hormone-producing gland, an over or underactive thyroid can be detrimental to one’s health. There are various thyroid diseases and conditions, including Hashimoto’s Disease, where the immune system confuses the thyroid for a foreign structure and attacks it, thinking it’s defending the body.
Treatment
When deciding whether HRT is the right treatment option for you, your GP will assess the severity of your symptoms, your age, lifestyle and personal and family medical history.
Lifestyle changes
There are a number of lifestyle changes you can make to help lessen your symptoms. Ensuring you exercise regularly, eat a well-balanced diet and get enough sleep is highly recommended and often helps improve symptoms. Furthermore, practicing relaxation methods such as breathing techniques, yoga or tai chi can help relieve menopausal symptoms related to moods, anxiety and stress. If you smoke or drink excessively, it is a good idea to stop, as this can increase the risk of heart disease, stroke, osteoporosis and cancer, whilst also increasing hot flashes.
Cognitive Behavioural Therapy (CBT)
CBT is a type of ‘talking therapy’ which helps alter the way people think, by attempting to change behaviours and recognise distorted ways of thinking. CBT is particularly useful as a treatment option for women who are experiencing mood swings, anxiety or depression as a result of the menopause.
Alternative methods
Some women prefer to seek relief through alternative methods such as acupuncture, rather than undergo HRT. Skeptics have argued that this only causes a placebo effect, but many doctors have confirmed that acupuncture can be a reasonable alternative where menopause symptoms are less severe and do not require medicinal treatment. Additionally, hypnotherapy as a treatment option has increased in popularity over the past few years.
BENEFITS OF HORMONE REPLACEMENT THERAPY (HRT)
Bioidentical hormone therapy (BHRT) is a safe and effective method of duplicating the natural hormones that the body is failing to produce.
Hot flushes and night sweats – HRT is the most effective treatment to alleviate hot flushes which can interfere with work and be very embarrassing. Night sweats can significantly affect the quality of sleep and leave women feeling tired and drained.
Bones – HRT is a very effective treatment for maintaining bone density if started before the age of 60. Preserving bone density is important in preventing osteoporotic fractures later in life. This is especially relevant as life expectancy is increasing. Oestrogen (estrogen) also helps the intervertebral discs in maintaining the collagen, and so prevent fractures of the vertebral bones.
Heart – there is good evidence that HRT started around the time of the menopause, prevents coronary heart disease and heart attacks in later life. This timing hypothesis is called ‘the window of opportunity’. Starting HRT below the age of 60 can reduce heart disease significantly, whilst starting HRT after the age of 60 can increase the risk.
Depression and mood – declining oestrogen levels are related to low mood and depression. Women who have previously suffered with premenstrual or postnatal depression are especially prone to experiencing cyclical depression in the 2-3 years leading up to the menopause. Oestrogen can be especially helpful in these cases.
Sexual function – declining oestrogen levels cause a reduction in collagen in the vaginal tissues leading to vaginal dryness and painful intercourse. In some cases, libido can be affected, caused by a reduction in androgen production by the ovaries, which is more pronounced in women who have surgery to remove the ovaries. The menopause can have an effect on the bladder, causing urgency, frequency and dysuria. These symptoms are part of genitourinary syndrome of menopause, which can be treated with systemic and local oestrogen.
Skin – as oestrogen levels fall, the collagen in the tissues reduces, leaving skin looking thin and dry. Oestrogen HRT can help retain the vitality of the skin.
Alzheimer’s and dementia – there is evidence that HRT started at the time of the menopause can reduce the risk of dementia in later life.
General wellbeing – many women with low estrogen report feeling more anxious and irritable, with tiredness and memory loss. HRT can significantly improve mood, and general function to allow you to continue to live good quality life.
HRT comes as tablets, gels, patches, implants and pessaries. The exact type of HRT suitable for individuals varies and a tailored approach allows for treatment of specific symptoms. A holistic approach incorporating HRT but also emphasising measures to promote general physical and mental wellbeing are key to optimal management of the menopause.
BIOIDENTICAL Hormonal replacement therapy

Oestrogel
What is Oestrogel?
Oestrogel contains the hormone 17 beta-oestradiol, which is the main type of oestrogen in our bodies. It is derived mainly from the yam, a root vegetable, and is a body identical type of HRT. It is packaged in a pump-action bottle called a ‘pump pack’, and each bottle has 64 pumps of oestrogen gel in it.
How do you use Oestrogel?
The most common dose for Oestrogel is between two and four pumps a day. Usually, if you need more than two pumps it is preferable to divide the doses for use in the morning and in the evening. It can be very common for younger women to need higher doses of Oestrogel and this is safe.
The gel should be rubbed into your skin on either the outside of your arms or the inside of your thighs. It is not greasy and does not have an odour. It does not usually stain clothes and most women find it dries easily.
Once your skin is dry, you can wear clothes and exercise normally. It is usually advisable to wait around 30 minutes before using other creams on the area, including sun cream.
You should wash your hands with soap and water after applying the gel.
How does Oestrogel work?
The gel is replacing the oestrogen hormone - the most important hormone for women that reduces during the perimenopause and menopause. In most cases, it effectively improves symptoms such as hot flushes, night sweats, mood changes and vaginal dryness.
If you still have your womb (uterus), you should also take a type of progestogen - either as a capsule, tablet or have the Mirena® coil inserted. A progestogen is needed to stop the lining of the womb building up, which can occur if only an oestrogen treatment is used.
What are the advantages of oestrogen gel compared to taking tablets?
The absorption of the gel is more reliable than taking it as a tablet because it goes straight into your bloodstream through your skin. There is no risk of blood clot using oestrogen as a gel, whereas there is a small increased risk when taking oestrogen as a tablet. In addition, women who have a history of migraines can still use oestrogen as a gel, in fact they should not take it in tablet form.
Many women enjoy the flexibility of changing the dose depending on their symptoms. Often people find that their need for oestrogen can increase or decrease with time; the dose of gel can alter accordingly. Changing the amount of gel you use should only be in consultation with your menopause doctor or GP.
Is Oestrogel the same as Oestrodose?
Some women find that when they have their prescription of oestrogen gel from another pharmacy, they receive Oestrodose, which is in a different container. Although these are made by the same company, some women find that Oestrodose is slightly less effective than Oestrogel. If you do notice a return of your symptoms you can obtain further Oestrogel from our clinic, or by using your NHS prescription at www.theindependentpharmacy.co.uk
Estradiol and Testosterone pellets

Hormone Subcutaneous Pellets for Women.....and Men
Hormone replacement therapy by pellet implantation has been used with great success in the United States, Europe and Australia since 1938. Pellets deliver consistent, physiologic levels of hormones and avoid the fluctuations of hormone levels seen with other methods of delivery. Estrogen delivered by subcutaneous implants maintains the normal ratio of estradiol to estrone.
Hormone pellets are safe, effective treatment for patients suffering from hormonal imbalances. Hormones delivered by the subcutaneous implants bypass the liver, do not affect clotting factors and do not increase the risk of thrombosis. Bioidentical testosterone delivered subcutaneously by pellets is also cardiac protective, unlike oral, synthetic testosterone. Testosterone and estradiol delivered by pellet implantation, does not adversely affect blood pressure, lipid levels, glucose or liver functions. Hormone replacement therapy with pellet implantation has an extremely low incidence of side effects and high compliance rate.
Hormone replacement therapy with estradiol and testosterone implants has been found to be superior to oral and topical (both the patch and gel) hormone replacement therapy for bone density. The pellets not only prevent bone loss but actually increase bone density. There is more data on hormone implants and bone density than any of the bisphosphonates (medication used to treat osteoporosis). Hormone replacement therapy with a 20 mg estradiol pellet has been shown to have a lower risk of breast cancer than patients without hormone replacement therapy. Even after over 20 years of therapy with hormone implants, the risk of breast cancer is not increased.
Pellets are superior to oral and topical hormone therapy with respect to relief of menopausal symptoms. Estradiol and testosterone implants have consistently been shown to improve insomnia, sex drive, libido, hot flashes, palpitations, headaches, irritability, depression, aches, pains, and vaginal dryness. It has also been shown to be effective in the treatment of migraine headaches.
Testosterone implants in both men and women have been shown to improve lethargy, depression, loss of libido, hot flashes without attenuating the beneficial affects of estradiol on cardiac and lipid profiles. Testosterone replacement therapy in men with subcutaneous implants (pellets) has been shown to be extremely effective, convenient and safe. Furthermore, FDA approval is required for ‘drugs being marketed to the public’. Pellets, in the United States are compounded and not ‘marketed to the public’.Testosterone delivered by subcutaneous pellet implants does not increase the risk of breast cancer as does oral, synthetic methyl-testosterone.
Vaginal dryness

Vaginal Dryness
VAGINAL DRYNESS: THE FACTS
Vaginal dryness can impact women, whatever their age, as a result of hormonal changes, anxiety, stress, cancer treatment, breastfeeding and side effects of some medications.
During perimenopause and menopause, the depleting oestrogen can lead to a thinning of the walls of the vagina and the skin of the vulva, making it shrink, feel sore, drier and less well lubricated. This can make sexual activity feel uncomfortable or painful and may lead to infections such as thrush, bacterial vaginosis and irritation.
The walls of the urethra that lead from the bladder also thin, leading to cystitis and urinary tract infections, as they become irritated and inflamed during penetrative sex.
Some women experience vaginal atrophy, which is much more than vagina dryness. It can lead to splitting or tearing of the vulva/vagina, constant itching, burning, soreness, discomfort and recurrent urinary issues which is why seeking medical advice to get the right diagnosis and treatment is important.
if symptoms aren’t well controlled on a 2x week regimen of vaginal oestrogen, I advise women they can increase the use to up to 5 x a week. Every woman has different symptoms & different response to treatment. Treatments need to be personalised.
I also frequently use Vagifem (Oestradiol ) and Ovestin (Estriol) together or on alternating nights. They work on different receptors within the vaginal tissue and can complement each other. Lots of pelvic floor physios have been advising this for years.