Tests During Pregnancy
Your First Test- a Positive Pregnancy Test!
Congratulations!
Learn about the importance of folate and Vitamin D during pregnancy, and potential complications during the first trimester here, or clicking on the image.
Other types of tests offered during your pregnancy are summarized below.
- Blood pressure checks- each visit
- Routine blood and urine tests- first visit before 10 weeks
- PAP smear- first visit before 10 weeks
- Glucose tolerance test for some - 28 weeks
- Vitamin D Level- optional. But some authorities recommend testing 3 times during pregnancy
- Combined first trimester screen- about 12 weeks
- NIPT testing-( optional genetic testing not through NHS) Anytime after 10 weeks
- Carrier screening (optional, not through NHS)- anytime during pregnancy or before pregnancy
- More on carrier screening
- More on NIPT testing
- Genetic Amniocentesis- specialized genetic test 16+ weeks
- CVS- specialized genetic test. 11-14 weeks
- Ultrasound scans.
A. Viability scan, before 11 weeks
B. Nuchal translucency first trimester screen 11-14 weeks
C. Fetal anatomy scan 18-22 weeks
D. 3rd trimester growth scan
Blood Pressure Checks
Blood Pressure Checks
Having regular checkups with blood pressure checks is one of the simplest but most important 'tests' you should do during your pregnancy. Checking your blood pressure regularly is especially important after 24 weeks.
If your reading is higher than normal, in many cases your next blood pressure reading will be normal. Even if it isn't, many pregnant women with high blood pressure deliver perfectly healthy babies, although it does require careful monitoring.
Be sure to let your practitioner know if you're concerned about any unusual symptoms, especially sudden weight gain or severe swelling, which could be signs of preeclampsia or more serious conditions
Routine Blood Tests During Pregnancy
Blood and Urine Tests
Testing and Screening may be slightly different between countries.
Initial Blood and Lab Tests in the U.S.
These tests are done at your first visit and include having a blood draw and giving a urine sample.
- Blood Count: To evaluate for anemia and count the platelets.
- Blood Type and Rh Factor: All Rh-negative moms will need Rhogam at 28 weeks to help prevent a rare condition known as HYDROPS, or fetal anemia.
- Rubella Status: We check your immunity to Rubella, so you may be vaccinated after pregnancy if necessary. Rubella infection during pregnancy can cause severe birth defects.
- RPR: RPR (syphilis) can cause devastating birth defects if not treated. Mothers can have syphilis and not know it. Treatment prevents the baby from getting syphilis birth defects.
- Hepatitis B: Children born to infected mothers can get this hepatitis and liver cancer. A vaccine to prevent Hepatitis B is given to ALL children. There is a special antidote given immediately after delivery to those babies born to mother what “have” hepatitis B.
- Gonorrhea and Chlamydia: These are common sexually transmitted infections that are universally tested in pregnancy. Babies born to infected mothers are at risk of blindness from eye infection.
- PAP Smear: Just like at your yearly exam…[read more]
- HIV: Testing for HIV is offered to all pregnant women, although it is not mandatory. We have medicines which prevent babies from getting HIV from mothers. Medicine reduces the chance of mother-baby transmission from about 33% to ALMOST ZERO.
- Urine Culture: Bladder infections (often without symptoms in pregnancy) can lead to kidney infections, and kidney infections are associated with early labor. Later in pregnancy, your urine is checked for several things, including protein which cann be a sign of pre-eclampsia.
From the MAMA Academy
The MAMA Academy was started by Heidi Eldridge, who lost her baby to stillbirth. Read her story here.
Glucose Tolerance Test (GTT)
This is a specific test to check for diabetes. Also called the OGTT (oral glucose tolerance test), this involves drinking a sugary drink and having blood tests. The OGTT is done when you're between 24 and 28 weeks pregnant. If you've had gestational diabetes before, you'll be offered:
- early self-monitoring of blood glucose levels, or
- an OGTT earlier in pregnancy, soon after your booking visit, and another at 24 to 28 weeks if the first test is normal
Reasons to have a GTT include:
- Having a BMI of over 30
- Asian origin
- Previous pregnancy with gestational diabetes
- Sugar in the urine (One high reading or two low readings)
- Previous baby weighing more than 4.5kgs
- Family history of diabetes
28 Week Bloods
Full Blood Count
Check for anemia. Hb – your haemoglobin (Hb) level is affected by your iron levels. In pregnancy it is normal to appear slightly anaemic. This is due to extra fluid present in the blood so the blood dilutes itself slightly. This corrects itself after pregnancy. Any Hb level below 10.5 should be treated with a low level of iron treatment and monitored.
Blood Group – to make sure no antibodies have developed during the pregnancy
PET Bloods
These are taken if you have high blood pressure, protein in your urine or both. They are checking your iron level, and kidney and liver function. (visit our High Blood Pressure page for more information)
Kidney function (U&E)
Your Urea and creatinine levels should be below the normal range for a non-pregnant person. This is again due to the extra fluid in the blood and due to dilution.
Liver function (LFT)
The only change here is that your ALP will be raised. ALP is a hormone released by the liver and your bones. It is also released by the placenta which is why it is normally raised in pregnancy and nothing to be concerned about.

Other Blood Tests to Consider
Vitamin D Level
First Trimester Screening
First Trimester Screening
Consider getting a vitamin D blood test from your provider or a home vitamin D test. Authorities in vitamin D and pregnancy actually suggest 3 levels during the pregnancy.
Vitamin D has now been shown to reduce the risk of a variety of pregnancy related complications, many of which can be traced to placental function.
- prematurity (preterm birth)
- preeclampsia and fetal growth restriction
- gestational diabetes
- possibly reduce the risk of miscarriage
- contributes to the regulation of placental inflammation.
- reduce the risk of autism, both in animal and human studies
First Trimester Screening
First Trimester Screening
First Trimester Screening
At the time of a 12 week (11 to 13+6) weeks) nuchal translucency (NT) ultrasound scan (offered to all pregnant women), you will also be offered a blood test measuring human chorionic gonadotropin (HCG), which tends to be increased in affected fetuses, and plasma associated protein A (PAPPA) which tends to be decreased in affected fetuses with Down syndrome. This test is offered as standard through the NHS. It can detect approximately 85% of major chromosome abnormalities like fetal Down syndrome, but there is also at least a 5-7% chance of a false positive result, in which case genetic amniocentesis or CVS might be suggested.
NIPT Testing
Carrier Screening
Carrier Screening
NIPT (non invasive prenatal testing) is a specialized genetic test of the fetal DNA, usually taken at 10-13 week range. These tests directly analyze fetal DNA fragments circulating in the maternal circulation. They are highly accurate for detecting fetal trisomy 21 (Down Syndrome) and other major chromosome abnormalities. The advantage is both the higher detection rate (99.5%) and the very low false positive rate (less than 0.5%). However, NIPT tests and cost vary with the extent of testing. They are offered to some selected high risk patients in the NHS.
There are 3 types of NIPT tests
- A standard NIPT test identifies 99.5%, of fetuses with trisomy 21 (Down syndrome),97% of fetuses with trisomy 18 (Edwards syndrome) and 92% of fetuses with trisomy 13 (Patau syndrome).
- Intermediate NIPT tests evaluate the basics (trisomies 21, 13 and 18) as well as selected microdeletions, including DiGeorge syndrome (q22 del)
- Comprehensive or Genome wide NIPT tests evaluate all parts of all chromosomes. This is a more intensive laboratory procedure and so more expensive, and not offered by all labs.
Carrier Screening
Carrier Screening
Carrier Screening

Carrier Screening
In addition to major chromosome abnormalities, a number of inheritable conditions with much smaller chromosome abnormalities may affect the baby. These are not detected with typical chromosome screening, but can be suspected based on carrier screening of the mother. These are typically x linked conditions or autosomal recessive conditions, so the mother may carry the gene even when she is perfectly normal. Because this is carrier screening of the mother, these tests can be performed any time, even before pregnancy. The most important of these conditions which parents might consider screening for include
More extensive panels can screen for over 100 conditions, many of them metabolic conditions which are otherwise not found until after birth when the baby begins feeding.
Carrier screening is routinely offered in the U.S., but is not routinely offered in the U.K.
More on Carrier Screening

More on Carrier Screening
Carrier Screening Recommended by ACOG
ACOG (American College of Obstetricians and Gynecologists) has updated two committee opinions on carrier screening. Committee Opinion 691 reviews the recommendations based on disorders. Committee Opinion 690 addresses the issues related to use of screening strategies such as expanded gene panel testing.
Changes to look for compared to previous guidance include the following:
- Spinal Muscular Atrophy (SMA) has now joined cystic fibrosis (CF) as a recommendation for all women who are pregnant or considering pregnancy
- Hemoglobinopathies
- Test all patients for CBC and RBC indices as part of antepartum care (ideally preconception)
- Add Hgb electrophoresis if:
- Increased risk based on ethnicity: African, Middle Eastern, Southeast Asian, West Indian and Mediterranean ancestry
- MCV is less than 80 fL with normal iron studies
- Ashkenazi Jewish Testing (central and Eastern Europe descent)
- Recommended testing remains for 4 disorders
- Canavan; CF; Familial dysautonomia; Tay Sachs Disease
- Additional tests to ‘consider’ has been expanded to the following
- Usher syndrome, Familial hyperinsulinism, Joubert and Maple syrup urine disease in addition to Bloom/Gaucher/Fanconi anemia/ML4/Neimann-Pick disease
- Recommended testing remains for 4 disorders
- Tay Sachs Disease
- In addition to Ashkenazi Jews, offer if either partner is French-Canadian descent or Cajun
- Screening can be performed using DNA-based testing (mutation analysis) or hexosaminidase enzyme in serum or leuckocytes (leukocyte only with oral contraceptives)
- Enzyme testing picks up approximately 98% of carriers regardless of ethnicity
- Mutation analysis is highly effective in at risk populations – detection rate is limited in other populations
In contrast, the NHS has no position on carrier screening for all patients. Instead, they suggest talking to your GP is there is a history in your family.
Speak to your GP if you're planning a pregnancy and:
- you've had a child with SMA before
- you have a history of the condition in your family
- your partner has a history of the condition in their family.
More on NIPT Testing

More on NIPT Testing
From the Fetal Medicine Centre
What is trisomy 21, 18 or 13?
In humans, there are 23 types of chromosomes and most people have a pair of each one of these chromosomes (therefore a total of 46 chromosomes). In trisomy, there are three rather than two of a particular chromosome (total of 47 chromosomes). The most common trisomies are those of chromosomes 21, 18 and 13.
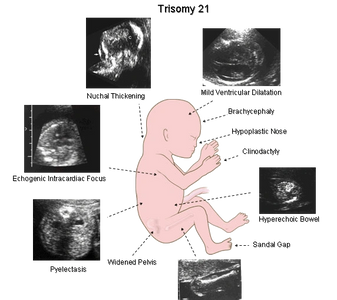
- Trisomy 21 is found in about 1 in 700 births and the risk increases with maternal age. The condition is associated with intellectual disabilities and some physical defects, most commonly heart abnormalities. The life expectancy is now about 60 years, if survival beyond the neonatal period.
- Trisomies 18 and 13 are found in about 1 in 7,000 births and the risk increases with maternal age. The conditions are associated with severe mental handicap and several physical defects. Most affected individuals die before or soon after birth and they rarely survive beyond the first year of life.
When do I expect to get the results?
- The results from the test will generally be available within 5-7 days, sometimes sooner.
- In about 3% of cases the test does not give a result, resulting in a failed test. This is due to technical problems with the analysis of the sample and does not suggest that there is a problem with the baby. If you want you can have the test repeated (at no cost) and in most cases the repeat test will show a normal result. It is important to ensure that the fetus is alive and developing normally by ultrasound, especially when the first test fails.
What will the results show?
- If the NIPT test shows that there is a high risk that the fetus has trisomy 21 or 18 or 13 you should consider confirmation with another test. CVS (chorionic villus sampling) or amniocentesis are considered definite tests to confirm a chromosome abnormality. If the ultrasound shows a definite abnormality- such as large nuchal translucency, or structural abnormality- AND the NIPT test is positive, then that also indicates a very high probably of an affected fetus.
- If the NIPT test shows that there is a low risk (less than 1 in 10,000) that the fetus has trisomy 21 or 18 or 13 it is unlikely that the fetus has one of these defects.
Do I need to have any other tests?
- A standard NIPT test does not provide information on other rare chromosomal abnormalities. Only the Genome test evaluates all parts of all chromosomes. If the scan at 11-13 weeks shows a high nuchal translucency (more than 3.5 mm) or major defects, such as exomphalos, holoprosencephaly, heart abnormalities or megacysis, the risk for some rare chromosomal defects is high. In such cases you may choose to have CVS or amniocentesis.
- Nuchal translucency evaluation by ultrasound may be helpful, even when your NIPT test is normal.
- A high quality ultrasound performed at 18-22 weeks remains the single best prenatal test to ensure the baby and pregnancy are developing normally. NIPT tests do not provide information on physical defects with normal chromosomes, such as heart or brain abnormalities and spina bifida, or fetal growth. All women should have an ultrasound scan at 18-22 weeks to examine the fetal anatomy (and also look at other important areas like the cervix) and should consider a scan at 28-32 weeks to evaluate fetal growth.
NIPT Testing
A video from Illumina - one of the laboratories which performs NIPT testing- to explain the science behind it.
Genetic Testing: Genetic Amniocentesis

Genetic Amniocentesis
Amniocentesis is a very specialized test, usually performed a a genetic test. It is considered the most accurate method of testing fetal chromosomes (and sometimes other things) but carries a small risk of losing the pregnancy.
From the Fetal Medicine Centre
What is amniocentesis?
- Amniocentesis involves the examination of cells in the fluid from around the fetus (amniotic fluid).
The cells in the amniotic fluid originate from the baby and so the chromosomes present in these cells are the same as those of the baby.
How is amniocentesis done?
- Amniocentesis involves passing a thin needle into the uterus in order to remove a small volume of amniotic fluid. The needle is carefully observed using ultrasound scan.
- The fluid is fetal urine and the amount removed by amniocentesis reaccumulates within a few hours.
- The procedure lasts 1 minute and afterwards we check that the fetal heart beat is normal.
What should I expect after amniocentesis?
- For the first couple of days you may experience some abdominal discomfort or period-like pain. You may find it helpful to take simple painkillers like paracetamol.
- If there is a lot of pain, bleeding, loss of fluid from your vagina or if you develop a temperature please seek medical advice.
When can I expect to get the results?
- The results for Down's syndrome and other major chromosomal defects are usually available within 3 days. The results for rare defects take 2 weeks. As soon as we get the results, we will call you to let you know
What are the risks associated with amniocentesis?
- The risk of miscarriage due to amniocentesis is about 1% and this is the same as the risk from chorion villus sampling. If you were to miscarry due to the test, this would happen within the next five days.
- Some studies have shown that when amniocentesis is performed before 16 weeks there is a small risk of the baby developing club feet. To avoid this risk we never perform amniocentesis before 16 weeks.
Chorionic Villus Sampling

Chorionic Villus Sampling
Choronic Villus sampling is an alternative specialized genetic test, similar to amnioctensis, but it can be performed earlier. Instead of sampling the fluid around the baby, CVS samples the placenta (which forms from the same DNA that makes the baby)
From the Fetal Medicine Centre
What is chorion villus sampling?
- Chorion villus sampling (CVS) involves the examination of chorionic villi (placental tissue). Both the baby and placenta (afterbirth) originate from the same cell and so the chromosomes present in the cells of the placenta are the same as those of the baby.
How is CVS done?
- Local anaesthetic is given. A fine needle is then passed through the mother's abdomen and a sample of villi is taken. The needle is carefully observed using ultrasound scan.
- The procedure lasts 1 minute and afterwards we check that the fetal heart beat is normal.
What should I expect after the CVS?
- For the first couple of days you may experience some abdominal discomfort, period-like pain or a little bleeding. These are relatively common and in the vast majority of cases the pregnancy continues without any problems.
- You may find it helpful to take simple painkillers like paracetamol.
If there is a lot of pain or bleeding or if you develop a temperature please seek medical advice
When can I expect to get the results?
- The results for Down's syndrome and other major chromosomal defects are usually available within 3 days. The results for rare defects take 2 weeks. As soon as we get the results, we will call you to let you know.
Will the procedure need to be repeated?
- In approximately 1% of cases the invasive test will need to be repeated because the results are inconclusive.
What are the risks associated with the test?
- The risk of miscarriage due to CVS is about 1% and this is the same as the risk from amniocentesis at 16 weeks. If you were to miscarry due to the test, this would happen within the next five days.
- Some studies have shown that when CVS is performed before 10 weeks there is a small risk of abnormality in the baby's fingers and/or toes. To avoid this risk we never perform CVS before 11 weeks.
Ultrasound Scans During the Pregnancy- 4 routine times
20 Week Fetal Anatomy Scan
20 Week Fetal Anatomy Scan
20 Week Fetal Anatomy Scan

At about 20 weeks, you should have an ultrasound scan which will look at baby 'head to toe' and confirm everything is developing normally.
This is also the time to look at the cervix which acts like a 'plug' to hold the pregnancy in the uterus (womb). More on preterm births and prevention here.
3rd Trimester
20 Week Fetal Anatomy Scan
20 Week Fetal Anatomy Scan
The third trimester is the best time to confirm that baby is growing normally and appears healthy. This may not be offered to all patients in the NHS. Review the GAP protocol criteria below to see if you have a risk factor and should request a scan.
More on potential complications of third trimester pregnancy here.
Common Ultrasound Issues

Low Lying Placenta
Placental position is determined by ultrasound. The placenta is most often in the front (anterior) or back (posterior) of the uterus, but also may be on the sides or at the top.
It is common for a placenta to appear in a low position early in pregnancy, at the time of the fetal anatomy scan. Low is considered to be within 2 centimeters of the cervical opening.
If the placenta is more than 2 cm away on any ultrasound measurement, there is no placenta previa. If within 2 cm, you should be followed. Most low lying placentas seen at 20 weeks will resolve by 30 weeks.
If the placenta is still low at 28 weeks-30, the next ultrasound is usually performed about 32-35 weeks. If it's still low or covering the cervix near the time of delivery, then you are likely to give birth by cesarean delivery, usually between 37 and 38 weeks. The timing of delivery is moved earlier based on the vaginal bleeding: how much and how recent. .
Ultrasound Potential Markers
There are a number of potential nonstructural or minor markers which may be seen at the time of the fetal anatomic scan around 20 weeks. These findings may sometimes indicate an underlying chromosome abnormality, like Down syndrome or other fetal abnormality, but are most often seen as a normal variant. As an isolated finding, these findings usually do not significantly change the risk. For additional reassurance, you might choose an NIPT test to confirm the chromosomes are normal.
These include:
- Echogenic intracardiac focus- a bright spot of spots, usually in the left ventricle. Most often seen in normal fetuses (2-3%), and even more common among Asians (up to 10%). Seen in about 30% of fetuses with trisomy 21 (Down syndrome) and 40% of trisomy 13.
- Choroid plexus cysts- fluid spaces within the choroid. The choroid are gland like structures located in the lateral ventricles of the brain, and secretes cerebrospinal fluid. These always go away by 22-24 weeks, even among fetuses with chromosome abnormalities. Seen in 1-2% of normal fetuses, up to 10% of fetuses with Down syndrome and 40% of those with trisomy 18.
- Renal pyelectasis- extra fluid within the collecting system of the kidneys. This is a common normal variant, seen more often in male fetuses compared to females. It occasionally is a sign of fetal Down syndrome but, if not normal, is more likely to indicate an underlying urinary abnormality.
- Short femur/ humerus. Like the other soft markers, this is usually seen in normal fetuses but may increase the risk for fetal Down syndrome. The incremental risk is very small. More often, short femur/ humerus may be associated with future growth delay or restriction. Evaluation should include Doppler of the uterine arteries. I would also suggest checking vitamin D levels.
- Nuchal thickening. This has the strongest positive predictive value for fetal Down syndrome among the potential soft markers that may be seen during the 2nd trimester, increasing the risk perhaps as much as 10 x. However, it is not sensitive, seen in less than 20%% of fetuses with Down syndrome. Care should be taken not to get an oblique view of the nuchal fold as this will over estimate true nuchal thickening Head compression with dolicocephaly will also increase the nuchal fold.
- Single umbilical artery- seen in 1 in normal 200 pregnancies, this is when there is a single umbilical artery rather than the normal paired two arteries. This may be seen in fetuses with trisomy 13 or 18, but those fetuses always show additional abnormalities. There is also a weak association with lower growth in the 3rd trimester for some fetuses.
Patient Downloads
Amniocentesis and CVS from RCOG (pdf)
DownloadMaterniT-GENOME-patient-brochure_Rep-1038 (pdf)
DownloadCarrier Screening brochure (pdf)
DownloadHarmony-test (pdf)
DownloadFragile X Syndrome -Carrier screening (pdf)
DownloadSpinal Muscular Atrophy (SMA) - carrier screening (pdf)
Downloadcystic fibrosis carrier screening (pdf)
Download