pelvic pain
Pelvic Pain
Pelvic pain is common- virtually all women will experience this at some time during their life. Fortunately, the causes are usually not dangerous and are often self limiting. When persistent, it is important to diagnose the underlying cause. Our goal is to first ensure the correct diagnosis, and then to offer the best treatment options to maintain or restore your good health. Although certainly ovarian cysts are the most common cause of sudden pelvic pain, there are other considerations.
In general, uterine causes are more likely to be the cause of abnormal bleeding while ovarian causes are more likely to be the cause of pelvic pain, but overlap occurs. Uterine pain is generally described as crampy. Fibroids may cause crampy pelvic pain. Adenomyosis is a uterine condition that can characteristically causes both abnormal bleeding and pelvic pain.
In women who are not pregnant, causes of pelvic pain to consider include:
- Ovarian cysts- described below.
- Endometriosis- a chronic, long-term condition where the tissue which lines the womb grows outside of the uterus and causes frequent pain, particularly during menstruation.
- Uterine cause- fibroids, adenomyosis
- Pelvic Inflammatory Disease (PID) – which are bacterial infections in the womb, often occurring as a result of a sexually transmitted infection, particularly Chlamydia or Gonorrhoea. PID requires immediate treatment via antibiotics, as leaving it untreated can lead to infertility.
- Urinary Tract Infection (UTI) – an infection of the urinary system which causes a painful burning sensation when using the toilet, or the need for frequent urination.
- Constipation – which causes pain in the abdomen and normally occurs because of dietary changes, some medications
- Irritable Bowel Syndrome (IBS)–a common long-term condition with symptoms that may include bloating, abdominal (stomach) cramps, constipation and diarrhoea.
- Chronic interstitial cystitis- which is a long-term condition where the bladder is inflamed.
- A hernia – which means an internal body part has pushed through into the muscle or tissue wall surrounding it
- Appendicitis – where the appendix swells up. This is normally very painful on the right-hand side of the lower abdomen.
- Peritonitis – which is the inflammation of the peritoneum; the tissue which lines the inside of the abdomen. Symptoms are sharp, sudden pain in the abdomen which slowly gets worse. Immediate treatment is vital.
When to see a doctor
In most cases, pelvic pain is caused by benign conditions which are non-cancerous, but that is not to say that pelvic pain which is not cancer-related cannot still be serious. Other conditions that cause sudden, severe pelvic pain, like ectopic pregnancy or appendicitis, need to be dealt with as a matter of urgency, as they can be life-threatening.

Chronic pelvic pain
Chronic Pelvic Pain
Chronic pelvic pain (six months or longer) can have multiple causes. It can be a symptom of another disease, or it can be a condition in its own right.
Some causes of chronic unexplained pelvic pain include:
- Endometriosis. Chronic pelvic pain is highly suspicious for endometriosis. In my experience, this is particularly true with a retroverted uterus (which could contribute to retrograde menses flow of blood). Endometriosis can lead to scarring and adhesions.
- Musculoskeletal problems. Conditions affecting your bones, joints and connective tissues (musculoskeletal system) — such as fibromyalgia, pelvic floor muscle tension, inflammation of the pubic joint (pubic symphysis) or hernia — can lead to recurring pelvic pain.
- Chronic pelvic inflammatory disease. This can occur if a long-term infection, often sexually transmitted, causes scarring that involves your pelvic organs.
- Ovarian remnant/ post surgery. After surgical removal of the uterus, ovaries and fallopian tubes, a small piece of ovary may accidentally be left inside and later develop painful cysts.
- Irritable bowel syndrome. Symptoms associated with irritable bowel syndrome — bloating, constipation or diarrhea — can be a source of pelvic pain and pressure.
- Painful bladder syndrome (interstitial cystitis). This condition is associated with recurring pain in your bladder and a frequent need to urinate. You may experience pelvic pain as your bladder fills, which may improve temporarily after you empty your bladder.
- Pelvic congestion syndrome. Some doctors believe enlarged, varicose-type veins around your uterus and ovaries may result in pelvic pain. However, other doctors are much less certain that pelvic congestion syndrome is a cause of pelvic pain because most women with enlarged veins in the pelvis have no associated pain.
- Psychological factors. Depression, chronic stress or a history of sexual or physical abuse may increase your risk of chronic pelvic pain. Emotional distress makes pain worse, and living with chronic pain contributes to emotional distress. These two factors often become a vicious cycle.
What you need to know
- Up to half of all women with chronic pelvic pain in secondary care have no obvious underlying pathology
- For pain relief, a combination of drugs, physiotherapy, and cognitive behavioural therapy can be tried
What are some methods used to relieve chronic pelvic pain?
Several pain-relief measures can be used to treat chronic pelvic pain. They include medications, physical therapy, nutritional therapy, and surgery:
- Lifestyle changes—Good posture and regular exercise may help reduce pelvic pain.
- Pain-relieving drugs—Nonsteroidal antiinflammatory drugs (NSAIDs) are helpful in relieving pelvic pain, especially dysmenorrhea.
- Physical therapy—Acupuncture, acupressure, and nerve stimulation therapies may be useful in treating pain caused by dysmenorrhea. Physical therapy that eases trigger points may give relief of muscular pain. Some types of physical therapy teach mental techniques for coping with pain. Such types include relaxation exercises and biofeedback.
- Nutrition therapy—Vitamin B1 and magnesium may be used to relieve dysmenorrhea.
- Surgery—Pelvic pain that does not respond to other treatments can be relieved by surgery. Cutting or destroying nerves blocks pain signals from reaching tissues and organs.
- Some drugs such as gabapentin might be useful
- Elagolix (Orilissa, AbbVie) is another drug that was approved in 2018 as an oral treatment for endometriosis-related pain. This medication is a gonadotropin-releasing hormone receptor antagonist that works by suppressing levels of hormones, including estrogen and progesterone. This helps decrease inflammation and the proliferation of endometrial tissue.

Types of Ovarian Cysts
Realize most ovarian cysts do not cause symptoms of pelvic pain, and so women are not aware they have them. However, other types of cysts- especially hemorrhagic cysts- may produce severe sudden pain which brings patients to A & E. The pelvic pain of hemorrhagic cysts can be scary at the time- but hemorrhagic cysts are self limiting, and resolve within 6 weeks (with significant resolution and improvement in symptoms often within 1 week).
Types of Ovarian / Adnexal Cysts
- Functional Cysts
- Follicles
- Dominant follicle/ simple cyst
- Anovulatory follicle/ cyst
- Hemorrhagic cyst
- Paraovarian/ peritubal cyst
- Endometrioma/ endometriosis
- Tubal (hydrosalpinx, hematosalpinx, pyosalpinx)
- Pseudocyst (loculated peritoneal fluid with adhesions)
- Benign Ovarian Tumors
- Cystadenoma
- Dermoid cysts
- Other benign tumors
- Malignant Ovarian Tumors (Cancer)
Types of Ovarian Cysts by Ultrasound: Simple vs Non Simple
From an ultrasound perspective, I separate cysts into 2 primary groups
1. Simple or nearly simple cysts-
We generally don't worry about these regardless of the cause, but will follow persistent cysts. Possible causes include:
- Functional Cyst
- Paraovarian/ peritubal cyst
- Tubal (Hydrosalpinx)- may be confused for ovarian cyst
- Benign Tumors
- Cystadenoma
2. Non simple or echogenic cysts
All other types of cysts may be non-simple (may be described as echogenic, septated or complex). The most common are hemorrhagic (or partially hemorrhagic) functional cysts vs. endometriomas. Hemorrhagic cysts typically show prominent peripheral vascularity and resolve in 6 weeks, whereas endometriomas are usually avascular and persist. Dermoid cysts are also common and may sometimes be difficult to distinguish from an endometrioma. Finally, we have to consider non- benign or malignant ovarian tumors
Non Simple Cysts
- Functional Cysts
- Hemorrhagic cyst- resolve within 6 weeks
- Paraovarian cyst- rarely hemorrhagic
- Endometriomas
- Tubal (hematosalpinx, pyosalpinx)
- Pseudocyst (loculated peritoneal fluid with adhesions)
- Benign Tumors
- Dermoid cysts
- Other benign tumors
- Malignant tumors (Cancer)

Simple Ovarian Cyst
Types of Ovarian Cysts- Ultrasound Appearance
Functional ovarian cysts
Functional ovarian cysts
Functional ovarian cysts

Ovarian cysts are very common, and functional cysts are by far the most common cause. In premenopausal women, a dominant cyst, or corpus luteum, forms with each cycle. Usually these cysts are small- 2 to 3 cm before ovulating. Functional cysts usually resolve quickly- usually within 6 weeks.
Simple ovarian cyst
Functional ovarian cysts
Functional ovarian cysts

Simple ovarian cysts are common. They are most often dominant follicles which have become larger than usual (dominant follicles usually ovulate less than 3 cm in size). Simple cysts may also be anovulatory follicles. The cysts may become much larger and do not release an egg (anovulatory cysts). This may persist several months and interfere with the normal cycle.
Hemorrhagic cysts
Functional ovarian cysts
Non functional cysts

Hemorrhagic cysts can produce severe, acute pain and women may seek help in A & E for their pain. Hemorrhagic cysts are not typically dangerous, however, and are self limiting. Hemorrhagic cysts usually occur when blood vessels surrounding the ovary rupture at the time of ovulation. Surgery always should be avoided for functional or hemorrhagic cysts, except for (rare cases) of life threatening hemorrhage.
Non functional cysts
Non functional cysts
Non functional cysts

Another type of nonfunctional cyst is a paraovarian or peritubal cyst. These also typically persist without change.
Dermoid
Non functional cysts
Ovarian Cancer

Most ovarian tumors are benign. Among these, the most common is a dermoid, or dermoid cyst. Most dermoids are entirely asymptomatic- women are not aware they have them. They are usually discovered during a pelvic exam or a pelvic ultrasound performed for other reasons. However, some tumors, like dermoids, may be associated with pelvic pain if they cause torsion, or partial torsion of the ovary.
Ovarian Cancer
Non functional cysts
Ovarian Cancer

Fortunately, ovarian cancer is much less common than the many benign conditions that may affect the ovary. Unfortunately, however, ovarian cancer usually does not produce pain or bleeding. If it did, we would discover it earlier. Instead, ovarian cancer has been called the 'silent killer' because of the lack of symptoms in early stages of the disease. So, women with pain and/ or bleeding usually do not have to be worried about ovarian cancer, even though it may be something many women consider. In later stages, the typical symptoms are pelvic discomfort with abdominal distension due to build up of fluid within the abdominal cavity.
We offer screening for ovarian cancer with ultrasound and blood tests.
Polycystic Ovarian Morphology/ Syndrome
Polycystic Ovarian Morphology (PCOM) or Syndrome (PCOS)
Polycystic ovarian syndrome (PCOS) is a common hormonal condition and deserves special mention. Patients with PCOS have a hormonal imbalance that can result in irregular periods, few periods (oligomenorrhea) or no periods (amenorrhea). They have high levels of Luteinizing hormone (LH), which leads to anovulation, and may lead to high levels of insulin and testosterone, Patients may have hirsuitism (excess hair growth) and acne. The typical 'cysts' are multiple small follicles, usually less than 10 mm, arranged in a peripheral location. Patients with PCOS may have superimposed other conditions including symptomatic functional cysts, so the presentation is not always clear.
- PCOS is common, affecting at least 15% of women of reproductive age.
- One of the central hallmarks of PCOS is an ultrasound scan showing typical findings of multiple small follicles, which can be termed polycystic ovarian morphology (PCOM). In about half the cases, the ovaries will also be enlarged.
- There is good evidence that many patients with PCOM but without clinical signs of PCOS are in a pre clinical phase.
- PCOS precede serious medical complications including type 2 diabetes and cardiovascular disease.
- Although there is no cure for PCOS, there is good evidence that early intervention with changes in diet and lifestyle can improve symptoms and help avoid some of the complications.

Typical PCOM
Videos-Polycystic Ovarian syndrome
A great video (see it on YouTube) explaining polycystic ovarian syndrome (PCOS)
CA 125 Blood Test
CA 125 Blood Test for Ovarian Carcinoma
CA125 blood test
Where there is a tumour present, the blood levels of the CA125 protein are often elevated, which could signal ovarian cancer. As such, this blood test is used to help determine whether an ovarian cyst could be cancerous. However, elevated CA125 levels can also occur in non-cancerous conditions, such as endometriosis, uterine fibroids and pelvic inflammatory disease. Also, ultrasound is more sensitive than CA 125 levels for detection of ovarian carcinoma. Therefore, CA 125 levels are best for watching changes over time, especially in cases considered to be intermediate risk based on ultrasound.
Other Ovarian/ Adnexal causes of Pelvic Pain
Endometriosis
Ectopic Pregnancy
Ovarian Torsion
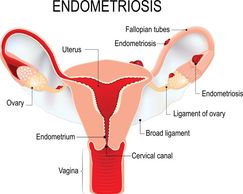
Endometriosis occurs when the cells of the uterine lining (endometrium) become dislocated around the ovary. This produces recurrent (chronic) bleeding, but the blood cannot escape and may produce pain.
Endometriosis may produce multiple tiny areas of hemorrhage which are difficult to impossible to visualize with ultrasound because of the small size. Larger areas of hemorrhage are termed endometriomas (chocolate cysts), and these may be readily visualized by ultrasound.
Ovarian Torsion
Ectopic Pregnancy
Ovarian Torsion

Occasionally, the ovary may twist or 'torte' on it's pedicle. This may stop the blood supply to the ovary, producing ischemia and severe pain. The ovary quickly enlarges. It's important to make a correct diagnosis so the ovary can be saved.
Ectopic Pregnancy
Ectopic Pregnancy
Hydrosalpinx/ pyosalpinx/ salpingitis

Ectopic pregnancy occurs when the pregnancy is located outside the normal location within the uterus, usually within the fallopian tube. Spotting or bleeding is often the first symptom but patients may also have pain or develop pain later. Most cases of ectopic pregnancy do not require surgery, but can be treated medically with methotrexate.
Hydrosalpinx/ pyosalpinx/ salpingitis
Hydrosalpinx/ pyosalpinx/ salpingitis
Hydrosalpinx/ pyosalpinx/ salpingitis

Hydrosalpinx is relatively common and usually asymptomatic. This occurs when the fallopian tube contains fluid, usually secondary to blockage of the tube. Superimposed infection causes inflammation (salpingitis) and may result in pyosalpinx (infected fallopian tube). This produce pain- sometimes severe- which usually can be treated with antibiotics.
Adhesions
Hydrosalpinx/ pyosalpinx/ salpingitis
Adhesions

Adhesions (scarring) may occur from prior surgery, infection, or conditions like endometriosis. Adhesions may sometimes produce loculations of peritoneal fluid, and these are often associated with pain. These loculations may mimic ovarian cysts, and so may be called 'pseudocysts'. They can be confused for ovarian cysts and even ovarian cancer to those who aren't familiar with this condition.
Videos-Endometriosis
A video explaining endometriosis