Fertilization

Fertilization
Fertilization (or fertilisation) is when a single sperm enters the egg with fusion of the DNA in each to form a new unique individual. This single cell develops into the embryo, and then a baby and finally birth. It's truly amazing. But how do we get there?
Normal fertility requires ovulation, introduction of sperm which travel to meet the egg, and then transport back down the fallopian tube to implant into a receptive endometrium and the amazing incubator called the uterus, or womb.
Not surprisingly, a number of issues can affect fertility. These include:
- Sperm count and quality
- Cervical mucous and cervical factors
- Maternal antibodies
- Ovarian reserve
- Ovulation
- Patency of the fallopian tube (for transportion of the sperm up the fallopian tube, and and the early fertilized pregnancy down the tube to the uterus)
- Endometrial receptivity
- Uterine malformations
- Other issues affecting the uterus or endometrium
Normal ovulation, fertilization,and early development

Normal Ovulation and Fertilization
Normal fertility is a complex process that first requires ovulation. Ovulation is itself a complex process. The sperm then need to make a perilous journey to reach the ovulated egg. As soon as a single sperm enters the egg, fertilization occurs. The fertilized egg must travel back down the fallopian tube and implant in the endometrium, 4-7 days later. It then quickly grows into the wall of the uterus with rapid cell division from a single cell to a very recognizable fetus just a few weeks later.

Changes in the Ovary and Endometrium
The normal cyclical changes in the endometrium and ovaries are a response to the cyclical change of hormones. Therefore, the ovaries and endometrium are highly synchronized normally. They may become unsynchronized in some situations.
In the ovaries, a number of follicles develop but a dominant ovulatory follicle becomes apparent. It becomes larger than the other follicles and usually ovulates by the time it reaches 18-30 mm in size. A surge in LH production by the anterior pituitary gland at approximately day 14 of the menstrual cycle stimulates the release of an egg from the dominant follicle and the formation of the corpus luteum.
Normal Ovulation and Menstrual Cycle
Normal Ovulation and Menstrual Cycle. Spectacular graphics
Cyclical Ultrasound Appearances of the Ovaries and endometriuM
Follicular phase
Follicular phase
Follicular phase

After menses and at the beginning of the next cycle, the normal ovary shows scattered follicles
Ovulatory Phase
Follicular phase
Follicular phase

The dominant follicle typically reaches a size of 18 to 30 mm before ovulation. The dominant follicle appears simple (black in current standard formatting).
Luteal phase
Follicular phase
Luteal phase
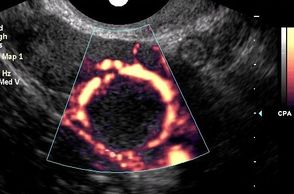
After ovulation, the dominant follicles no longer appears entirely black (simple). Instead, it shows internal echoes of hemorrhage and a mildly irregular and thickened wall. Prominent peripheral vascularity is also usually seen with Doppler studies.
Luteal phase

The endometrium is thinnest just after menses but then develops a proliferative, trilaminar pattern. The walls of the endometrium are relatively hypoechoic.

Near the time of ovulation, the endometrium becomes thicker but the walls are still hypoechoic, producing a trilaminar or proliferative pattern.

In the luteal phase of the ovary, the endometrium has developed a secretory pattern. The endometrium is now at it's thickest point and both walls are echogenic, reflecting many more interfaces due to vessels and mucosa. The central interface between the two walls remains intact.
The Corpus Luteum

The Corpus Luteum
On release of the egg, the ovulatory follicle becomes the corpus luteum. The corpus luteum releases progesterone, which prepares the body for pregnancy.
If the ovulated egg is fertilised and gives rise to an embryo, the cells that surround this early embryo (which are destined to form the placenta) secrete human chorionic gonadotropin (HCG). This hormone has a very similar chemical structure to LH. HCG can bind to and activate the same receptors as LH, and so maintains the corpus luteum which then continues to produce progesterone until the placenta is established.
If progesterone is absent or levels are too low, irregular and heavy menstrual bleeding can occur. A drop in progesterone during pregnancy can result in a miscarriage and early labour. Mothers at risk of giving birth too soon can be given a synthetic form of progesterone to delay the onset of labour.
Lack of progesterone in the bloodstream can mean the ovary has failed to release an egg at ovulation, as can occur in women with polycystic ovarian syndrome (PCOS).
The corpus luteum shows typical features on ultrasound. The corpus luteum is a thick walled cyst with characteristic "ring of fire" peripheral vascularity. It usually has a crenulated inner margin and internal echoes. Identification of a corpus luteum is evidence that ovulation has occurred. On the other hand, failure to demonstrate a corpus luteum suggests that ovulation has not occurred.
Ovulation and fertilization
Fertilization- truly a miracle!
Some things you just need to see to believe. We are all miracles. Creating a new life is a miracle.
Ultrasound Assessment of Infertility
Ultrasound Assessment of Infertility
High quality ultrasound can detect many abnormalities which can contribute to infertility including
- Polycystic ovarian syndrome
- Uterine malformations, such as septated uterus
- Fibroids (although not usually the cause of infertility unless intracavitary or submucosal)
- Polyps
- Endometriosis
- Decreased ovarian reserve
- Hydrosalpinx
In addition, a new contrast agent is available which is highly reliably for testing tubal patency, with accuracy similar to a hysterosalpinogram (which can be uncomfortable and requires ionizing radiation). This is critical information to help determine whether you should seek IVF help sooner.

Potential contributors to infertility seen by ultrasound
Uterine Malformations
Fibroids and Adenomyosis
Fibroids and Adenomyosis
Bicornuate uterus
Septate, subseptate
Uterine didelphys
Milder forms including arcuate
(click on image above for more detailed discussion)
Fibroids and Adenomyosis
Fibroids and Adenomyosis
Fibroids and Adenomyosis

Fibroids are common. Those closest to the cavity and especially those within the cavity are most likely to cause bleeding and contribute to infertility.
Importantly, Vitamin D deficiency may contribute to fibroids and Vitamin D has been found to be a powerful anti-fibroid and anti-tumour agen.
Endometrial Issues
Fibroids and Adenomyosis
Decreased Ovarian Reserve

Polyps- commonly missed elsewhere
Intracavitary fibroids
Adhesions
Other endometrial abnormalities including hyperplasia
Ablation and post ablation
Essure coils
Decreased Ovarian Reserve
Blockage of the Fallopian Tube
Decreased Ovarian Reserve

Decreased ovarian reserve may involve only a single ovary in some cases, or one ovary may have been surgically removed or partially removed. Decreased ovarian reserve in both ovaries may be seen from premature menopause or from chronic suppression by oral contraceptives.
Polycystic Ovarian Syndrome
Blockage of the Fallopian Tube
Blockage of the Fallopian Tube
Polycystic ovarian syndrome (PCOS) may cause irregular menses and contribute to infertility. In clinical practice, 75% of women with PCOS suffer from anovulation infertility and 50% of them experience recurrent pregnancy loss. It is, however, not clear whether these defects are caused by uterine dysfunction itself or by the interrupted interaction between uterine cells and the developing embryo.
Additionally, the chronic anovulation seen in PCOS implies prolonged estrogen excess or lack of progesterone and results in atypical endometrial hyperplasia, which is the precursor of endometrial carcinoma
Patients with PCOS also have a much higher chance of developing dermoid tumors
Polycystic Ovarian Syndrome

Polycystic Ovarian Syndrome
Polycystic Ovarian syndrome (PCOS)
- PCOS is common, affecting at least 15% of women of reproductive age.
- One of the central hallmarks of PCOS is an ultrasound scan showing typical findings of multiple small follicles, which can be termed polycystic ovarian morphology (PCOM)
- There is good evidence that many patients with PCOM but without clinical signs of PCOS are in a pre clinical phase.
- PCOS precede serious medical complications including type 2 diabetes and cardiovascular disease.
- Although there is no cure for PCOS, there is good evidence that early intervention with changes in diet and lifestyle can improve symptoms and help avoid some of the complications.
Fallopian tube conditions
Normal
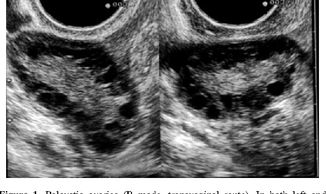
Infection
Infection

Normal pregnancy depends on a patent (open) fallopian tube for both transport of sperm up the fallopian tube near the ovary, and transport of the fertilized blastocyst down the tube toward the uterus.
Infection
Infection
Infection
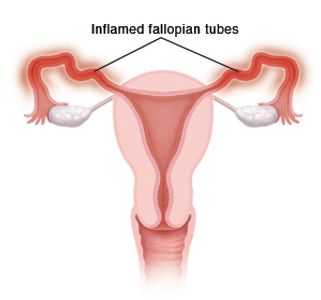
When the tube is infected, or inflamed, it may become enlarged and filled with fluid.
Hydrosalpinx
Endometriosis
Endometriosis

Blockage may be caused by endometriosis, prior infection, scarring, or unknown causes
Hydrosalpinx may be confused for ovarian cysts or other conditions
Endometriosis
Endometriosis
Endometriosis
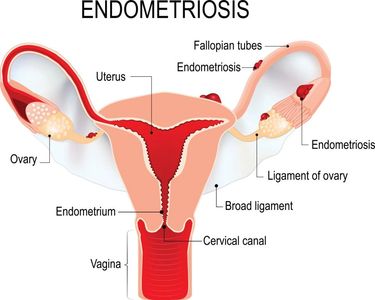
Endometriosis or infection may cause scarring of the fallopian tubes, resulting in blockage
Tubal Patency Studies
Tubal Patency Studies
Tubal patency –normal open fallopian tubes which allow transport of the sperm to the egg- is essential for natural pregnancy and fertility. Issues that can affect tubal patency include endometriosis, adhesions, and prior infection, but many women with tubal factors have no known cause. Abnormal fallopian tubes can be seen when dilated and filled with fluid (hydrosalpinx), which indicate the tubes are blocked. The fallopian tubes are otherwise not seen with standard ultrasound because normal tubes are too thin to see and they blend with adjacent structures.
Hysterosalpingograms (HSG) have traditionally been used to assess tubal patency. However, HSG requires ionizing radiation and contrast dye with X-ray technology. As a replacement for HSG, HyCoSy (hysterosalpingo Contrast Sonography) was developed. This technique has been widely utilized and has been found to be comparable to HSG. Hysterosalpingo-Foam Sonography (HyFoSy) represents a significant improvement to the older HyCoSy method. ExEm-gel creates a stable foam which last longer than liquid. This results in better images, more accurate results, and a more comfortable exam for the patient.
HiFoSy is an improvement on older methods, using a type of gel foam to visualize the tubes and assess tubal patency. The millions of tiny bubbles trapped in the foam produce a bright image on the ultrasound.
HiFoSy can be performed at the same time we evaluate the uterus and ovaries. The procedure is quicker, safer, more convenient, and with less discomfort compared to older procedures.
4 independent publications, involving 800+ patients, reported 30 – 46% spontaneous pregnancies within 2-6 months after HyFoSy Procedure using ExEm® Foam

HyFoSy Test for Tubal Patency
See the HyFoSy Test for Tubal Patency
What can you do?

Improving Fertility
- Address the underlying cause
- Although there is no cure for PCOS, there is good evidence that early intervention with changes in diet and lifestyle can improve symptoms and help avoid some of the complications.
- Don't smoke
- Omega 3s Fish oil has been associated with a long list of health benefits, and some research indicates that omega-3 supplements can decrease androgen levels in women with PCOS. One study found that women with PCOS who were given three grams of omega-3s a day for eight weeks had lower testosterone concentrations and were more likely to resume regular menses than subjects who received a placebo.
- Vitamin Supplementation, especially Folate (pre conceptional) and
- Vitamin D long term (see below)
- Don't hesitate to seek expert help
Vitamin D
Evidence suggests that vitamin D modulates human reproductive processes. Several observational studies reported a better in-vitro fertilization outcome in women with sufficient vitamin D levels (≥30 ng/ml), which was mainly attributed to vitamin D effects on the endometrium. One randomized controlled trial found an increased endometrial thickness in women with polycystic ovary syndrome (PCOS) receiving vitamin D during intrauterine insemination cycles. Further, vitamin D supplementation had a beneficial effect on serum lipids in PCOS women. Vitamin D treatment improved endometriosis in a rat model and increased vitamin D intake was related to a decreased risk of incident endometriosis. Vitamin D was also favorably associated with primary dysmenorrhea, uterine leiomyoma (fibroids), and ovarian reserve in late reproductive aged women.A number of studies also suggest that vitamin D is a powerful factor against fibroids, resulting in inhibition of tumor cell division and a significant reduction in its size, however, the exact role of this compound and its receptor in the pathophysiology of fibroids is not fully understood.
In women undergoing in-vitro fertilization, a sufficient vitamin D level (≥40 ng/ml) should be maintained. Vitamin D supplementation might improve metabolic parameters in women with PCOS. A high vitamin D intake might be protective against endometriosis and fibroids.
Vitamin D and pregnancy
Vitamin D has become increasingly recognized as a pluripotent regulator of biological functions above and beyond its classical effects on bone and calcium homeostasis. Expression of vitamin D receptor (VDR) for the active form of vitamin D, 1,25-dihydroxyvitamin D (1,25(OH)2D), as well as the 1α-hydroxylase enzyme that synthesizes 1,25(OH)2D (CYP27B1), has been reported for various tissues that can be broadly termed ‘barrier sites’, indicating that localized responses to vitamin D may be a key feature of these tissues. Prominent among these barrier sites is the placenta, acting as the interface between mother and fetus. Historically, the placenta was one of the first extra-renal tissues shown to be capable of synthesizing 1,25(OH)2D. Initially, this was linked to the rise in maternal serum 1,25(OH)2D that occurs at the end of the first trimester of pregnancy. However, the presence of VDR in the placenta suggests that vitamin D functions in tissue-specific fashion at the fetal–maternal interface . One possible explanation is that 1,25(OH)2D acts as a regulator of placental calcium transport, but a placental immunomodulatory function has also been proposed. Moreover, the rapid induction of VDR and CYP27B1 early in pregnancy suggests that vitamin D may play a more fundamental role in the process of conception, implantation and development of the placenta itself. Thus, in addition to the active immune cell function classically observed in the maternal decidua, trophoblast cells also appear to make a major contribution to the regulation of placental inflammation. The concept of vitamin D as a regulator of cellular motility and invasion is not novel and has been extensively reported in cancer states , where effects of vitamin D have been related to modulation of epithelial–mesenchymal transition (EMT) . Vitamin D deficiency in pregnant women has been shown to be associated with increased risk for pregnancy complications . These include preeclampsia , fetal growth restriction, small-for-gestational-age fetus , bacterial vaginosis and gestational diabetes mellitus. Maternal vitamin D deficiency has also been linked to adverse effects in offspring, including reduced bone density and childhood rickets, as well as increased risk of asthma and schizophrenia. Low levels of vitamin D appear to contribute to the risk of autism, according to a study published in Molecular Psychiatry: According to the researchers, women with low vitamin D levels at 20 weeks of pregnancy are more likely to have children with symptoms of autism. Children born to women who had low blood levels of vitamin D while pregnant more than double their risk of autism according to a study of more than 4,000 children in the Netherlands.
Uterine Malformations
Uterine malformations result from abnormal development. Uterine 'duplication' actually occurs from incomplete fusion of the paired Mullerian ducts which normally occurs between the seventh and ninth weeks of gestation. This results in a spectrum of abnormalities, depending on the degree of fusion. Some uterine anomalies such as uterus didelphys have been associated with pain, infertility, miscarriage, preterm delivery and even endometriosis. The good news is that despite the increased risk, most women with uterine abnormalities are able to become pregnancy and carry healthy babies to term.
Uterine Abnormalities
Normal
Arcuate Uterus
Arcuate Uterus
A normal uterus has a rounded top and a triangular shaped cavity with a single cervix.
The wall of the uterus is comprised of smooth muscle.
The central lining, or cavity, of the uterus is lined by a layer of cells called the endometrium.
The fallopian tubes rises from each side of the uterus near the top.
Arcuate Uterus
Arcuate Uterus
Arcuate Uterus

This term has been classically difficult to define but represents a mild form of a septal uterus. In it, the myometrium of the fundus (the top portion of the uterus, opposite of the cervix), dips inward into the uterine cavity. When defined as having a midline prominence of 1.5cm or less, the arcuate uterus was found to make up 70% of uterine abnormalities. Arcuate uterus does not have any obstetrical implications, meaning it has not been found to have an association with infertility or miscarriages. However, there may be an association with endometriosis. The reason for this is probably due to abnormal contractions, resulting in a higher chance of retrograde contractions, so endometrial cells may be propulsed backwards toward the ovary. Many women with arcuate uterus may be incorrectly informed they have a bicornuate uterus.
Septate Uterus
Arcuate Uterus
Bicornuate Uterus
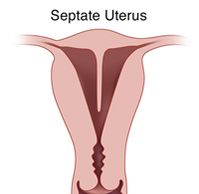
This malformation occurs when the uterine cavity is divided by a septum protruding from the fundus, but keeps the normal outer shape intact. A septate uterus is a common anomaly in women with a history of miscarriages and infertility. The septum is quite variable in length, but should be at least 1.5 cm. It forms a V shape, unlike the rounded U shape of an arcuate uterus. In some cases, the septum completely divides the uterine cavity and cervix into two halves. Resection of the septum can improve fertility and reduce the risk of preterm delivery for some patients.
Bicornuate Uterus
Unicornuate Uterus
Bicornuate Uterus
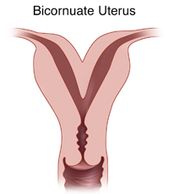
Bicornuate uterus appears similar to septated uterus, but the outer fundus no longer has the normal rounded shape. Instead, the outer shape shows a mid indentation at least 1cm and a wide intercornual (tube) distance that can be appreciated via hysteroscopy, as well as laparoscopy. A bicornuate uterus cannot be treated with simple resection and therefore surgery is not indicated. However, there is an increased risk of recurrent pregnancy loss, cervical incompetence, and preterm delivery. Many patients are told they have a bicornuate uterus when, in fact, they may have an arcuate uterus or septated uterus.
Bicornuate Uterus
Unicornuate Uterus
Unicornuate Uterus
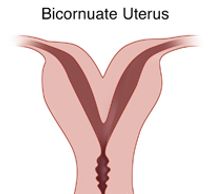
Bicornuate uterus appears similar to septated uterus, but the outer fundus no longer has the normal rounded shape. Instead, the outer shape shows a mid indentation at least 1cm and a wide intercornual (tube) distance that can be appreciated via hysteroscopy, as well as laparoscopy. A bicornuate uterus cannot be treated with simple resection and therefore surgery is not indicated. However, there is an increased risk of recurrent pregnancy loss, cervical incompetence, and preterm delivery. Many patients are told they have a bicornuate uterus when, in fact, they may have an arcuate uterus or septated uterus.
Unicornuate Uterus
Unicornuate Uterus
Unicornuate Uterus
This form of uterine anomaly occurs when the uterus is predominantly formed by just one of the two paired Müllerian ducts. This abnormality has been shown to have significantly greater chance of infertility, miscarriage, and preterm delivery. On coronal 3D images, the uterine cavity no longer shows a normal triangular shape, but rather assume a banana shape. However, unicornuate uterus is typically missed with standard 2D ultrasound. In part for this reason, all fertility patients should have 3D coronal images of the uterus.
3D Coronal IMAGES of Uterine Abnormalities
All of the uterine abnormalities described here can be seen with coronal 3D ultrasound, while they are often misdiagnosed, or even missed entirely with standard 2D ultrasound. Therefore, all fertility patients should have 3D scans of the uterus.


