Ultrasound Topics
Early Pregnancy
Miscarriage/ Non Viable Pregnancy
Ectopic Pregnancy
Pregnancy- Uterus, Placenta, Cervix, Ovaries
Pregnancy-Fetal: Soft Markers
Nuchal thickening
Shortened femur/ humerus
Pregnancy- 3rd Trimester Issues
Gynecologic- Uterine, Endometrial
Endometrial atrophy
Endometrial thickening
Gynecologic- Ovarian/ Adnexal
Ovarian cysts
Anovulatory cysts
Paraovarian cysts
Cystic neoplasm
Ultrasound Issues: The First Trimester

Miscarriage
The chance of miscarriage decreases dramatically after 9 weeks if the embryo is normal in size with a normal heart beat by ultrasound. If a heartbeat is present between 6 and 9 weeks, then there is still a chance of early miscarriage. Ultrasound findings of a nonviable pregnancy vary with the stage of pregnancy that was achieved. These include
- Embryo without a heartbeat. For additional certainty, it is suggested that the embryo size be more than 6 mm. However, this may not be necessary when other ultrasound findings are present, or when correlated with HCG levels or other information.
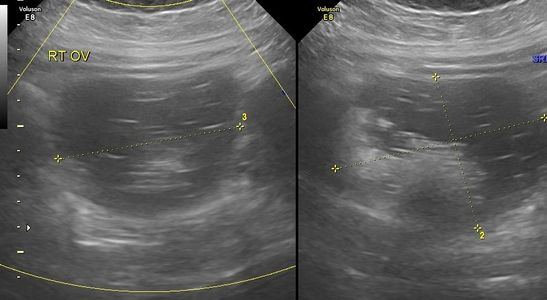
- Gestational sac with yolk sac but no embryo- the sac should be at least 20 mm unless other features are present
- Gestational sac with no yolk sac and no embryo- the sac should be at least 20 mm unless other features are present
- No gestational sac- if the gestational sac has already passed, or if the pregnancy never developed as far as a gestational sac (also termed a chemical pregnancy).
Other abnormal findings include irregular shape of the gestational sac, abnormal position (within the uterine cavity or low, indicating a miscarriage in progress), poor surrounding choriodecidual reaction, and abnormal internal morphology including an 'empty amnion'.
If the pregnancy is found to be nonviable, please remember 6 things, which you can find here or on the blog post
How to Know
Miscarriage diagnosis is often straightforward. In other circumstances the diagnosis requires multiple blood tests and ultrasounds.
Your Choices
WAIT & SEE: One may elect to let nature complete the miscarriage. The time course is not predictable. Miscarriage, passing tissue, can happen any day at any time. It may occur soon, or it can take weeks. There is no test to predict when it will happen.
Vaginal Pill: This pill is used to bring on a miscarriage. Once the miscarriage gets going, its just like a natural miscarriage, with all the bleeding and cramping. If the pill is going to do something it usually happens within six hours of taking the dose. A second dose can be taken the next day. Like wait and see, the pill can work, or not.
Surgery: When miscarriage is managed surgically, the cervix is dilated and the uterus is gently emptied with an instrument known as a Curette, known as a D&C. Surgery may be done for a few reasons:
- Nature is taking too long to complete the miscarriage.
- Nature can not finish the miscarriage, marked by persistent cramping and bleeding which is sometimes heavy.
- Patient prefers to schedule the procedure rather than waiting for the miscarriage to happen at home, or at work, or anywhere. Even when the miscarriage is completed at home, the bleeding and pain can be more than you expect.
When to Decide: There is No Medical Urgency in deciding what to do. A
What to Expect
A miscarriage is complete when the uterus is empty. The HCG (human chorionic gonadotropin, a hormone produced during pregnancy) will return to zero or negative.
Symptoms of Unfinished Miscarriage: Persistent cramping is highly suggestive of an incomplete miscarriage. Bleeding after a miscarriage can continue for 2-3 weeks, but it typically less than 10 days. The HCG blood test is not as reliable as cramping to determine if a miscarriage is finished and patients with persistent cramping need to make an appointment for evaluation. This may still happen, even after a D&C procedure.
Ectopic Pregnancy
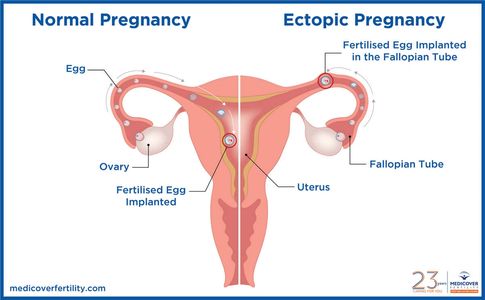
WHAT IS AN ECTOPIC PREGNANCY
Normal pregnancy is supposed to develop inside the uterus. Some women get pregnant but the pregnancy grows outside the uterus. A pregnancy which grows outside the uterus is called Ectopic Pregnancy. The most common place for such pregnancies to grow is in the fallopian tube.
Over time, ectopic pregnancy can become really dangerous. A woman can experience more and more pain, she may have internal bleeding, and she may need emergency surgery. While an ectopic pregnancy can not be prevented, it can be treated with medicine if the diagnosis is made early. The goal is early diagnosis and treatment, and avoiding surgery if possible.
Who’s at Risk
Women are considered at risk of ectopic pregnancy if they have already had:
- an ectopic pregnancy
- surgery to the fallopian tubes
- surgery to the colon
- a burst appendix
- chlamydia or gonorrhea
- PID (pelvic inflammatory disease)
- surgery for endometriosis with lots of scar tissue
Whatever caused a first ectopic pregnancy can cause a second. The chance of ANY woman having an ectopic pregnancy is approximately 1 in 100. The chance of a woman getting a SECOND ectopic pregnancy is approximately 1 in 20, and maybe as high as 1 in 3. Women who have ever had an ectopic pregnancy must be carefully evaluated in the first seven weeks of all pregnancies that follow. It is essential that any woman who had already had an ectopic pregnancy, and is now pregnant, contacts her OB/GYN for early pregnancy blood tests and ultrasounds, to diagnose or exclude ectopic pregnancy.
Confirming an Ectopic Pregnancy
Normal pregnancy is confirmed with an ultrasound seeing a fetus with a heartbeat in the uterus. The earliest we can find these things is 5 ½ weeks after the last period. All normal pregnancies can be confirmed at 7 weeks, based on ultrasound measurements of the fetus. Similarly, the diagnosis of an ectopic pregnancy is based on blood pregnancy tests and an ultrasound.
We can make the diagnosis of an ectopic pregnancy IF:
- we see a fetus in a sac outside of the uterus. This can be seen with ultrasound.
- the blood pregnancy test is rising over time but it does not rise fast enough or high enough.
- the blood pregnancy test is high enough, but an ultrasound doesn’t find a pregnancy in the uterus.
If You’re at Risk
Women at risk of ectopic pregnancy do extra home urine pregnancy tests IF:
- she feels pregnant.
- she does not have a period 5 – 6 weeks after the last period.
- the periods are irregular, a test should be done every six weeks.
Ultrasound Issues: Bleeding in Pregnancy

BLEEDING IN PREGNANCY: SUBCHORIONIC HEMORRHAGE
BLEEDING IN PREGNANCY
Many women will have some bleeding during pregnancy, especially in the first half of pregnancy. Here is a list of common reasons for bleeding during pregnancy, based on weeks of gestation.
To 13 Weeks
Bleeding is common. It almost always arises from the placenta or placental margin (occasionally from the cervix- Cervix infection and irritation can cause bleeding at any time in pregnancy). Placental bleeding may or may not form a subchorionic hemorrhage (SCH). Subchorionic hemorrhage may be very small and hard to visualize, or very large- even larger than the pregnancy. Older blood appears dark by ultrasound, more recent bleeding appears echogenic (brighter). What causes placental bleeding and subchorionic hemorrhage? Remember the placenta (which arises from baby) is attached to the uterus (you). Think of it as a special kind of glue. We want the glue to work well throughout pregnancy, but we want it to become unglued so the placenta can also deliver soon after birth of the baby. In the mean time, the uterus is growing, the placenta is growing, and the uterus has lots of contractions to help it grow. So...we are asking a lot from that special glue, and it's not surprising it can become unglued around the edges. The placenta is very vascular so any little bit of 'ungluing' is likely to result in bleeding.
Sometimes bleeding is a sign of miscarriage so it's best to make sure baby is ok with an ultrasound. If baby is ok, then there is little reason to worry, regardless.
From 13 Weeks to 18 Weeks
The same reasons for bleeding in the first 13 weeks of pregnancy can cause bleeding after 13 weeks, too. The cervix can still bleed, although less commonly. Bleeding from the subchorionic hematoma is usually dark, and is old blood, rather than new bleeding. NEW onset vaginal bleeding at this time in pregnancy should be evaluated with examination, including a speculum exam to see, and fingers to feel. Bleeding can be from the cervix opening up too soon.
Most bleeding issues occur in the first half of pregnancy. If it's isolated, there is no cause for concern. If it is continuous or recurrent, it may indicate underlying placental dysfunction and you may be at increased risk of 'placental related' complications during the 3rd trimester. I personally would check vitamin D levels and consider increasing supplementation.
From 18 Weeks to 34 Weeks
In the 18-22 range, vaginal spotting could be a sign of cervical dilatation due to incompetence and this should be evaluated. Bleeding from placenta previa is practically not as much of an issue because nearly all patients will already know about a low placenta from the ultrasound done at 20 weeks. Bleeding with pain is most commonly from labor, but can also be caused by early detachment of the placenta, or abruption. Placental abruption usually has heavier bleeding, more pain, and more constant pain. Bleeding from placenta previa is usually painless.
Between 34 and 37 Weeks
The most common cause of bleeding at this time in pregnancy is Premature Labor. As the cervix gets ready for labor, as it dilates, it can bleed. The dilation causes a mucousy discharge, which can be tinged red or brown, depending on how fresh the blood is. If the water bag breaks as the cervix dilates, fluid coming from the vagina can be red, mimicking heavy bleeding. We rarely stop a labor which starts after 34 weeks. Many babies born at this time in pregnancy will need extra medical attention at birth, so hospital evaluation is best. Placenta previa and placental abruption can also cause bleeding at this time.
After 37 Weeks
The most common cause of bleeding at this time in pregnancy is labor. The bleeding can be like the onset of a period. Light bleeding, without pain, can be managed just like the onset of labor. Heavier bleeding can still be labor, but patients should go in for evaluation sooner.

Low Lying Placenta/ Previa
Placenta previa happens in about 1 in 200 pregnancies, but it is diagnosed much more commonly in the first half of pregnancy before the lower uterus grows and stretches. This means that if ultrasound suspects placenta previa early in pregnancy, it usually isn’t a problem since most low lying placentas seen at 20 weeks will resolve by 30 weeks. Low is considered to be within 2 centimeters of the cervical opening. If within 2 cm, you should be followed.
If the placenta is still low at 28 weeks-30, the next ultrasound is usually performed about 32-35 weeks. If it's still low or covering the cervix near the time of delivery, then you are likely to give birth by cesarean delivery, usually between 37 and 38 weeks. The timing of delivery is moved earlier based on the vaginal bleeding: how much and how recent.
Normally, the placenta grows into the upper part of the uterus wall, away from the cervix. During the last stage of labor, the placenta separates from the wall, and your contractions help push it into the vagina (birth canal). This is also called the afterbirth.
If you have placenta previa, when the cervix begins to efface (thin out) and dilate (open up) for labor, blood vessels connecting the placenta to the uterus may tear. This can cause severe bleeding during labor and birth, putting you and your baby in danger.
Risk factors
Placenta previa is more common among women who:
- Have had a baby
- Have scars on the uterus, such as from previous surgery, including cesarean deliveries, uterine fibroid removal, and dilation and curettage
- Had placenta previa with a previous pregnancy
- Are carrying more than one fetus
- Are age 35 or older
- Are of a race other than white
- Smoke
Complications
If you have placenta previa, your health care provider will monitor you and your baby to reduce the risk of these serious complications:
- Bleeding. Severe, possibly life-threatening vaginal bleeding (hemorrhage) can occur during labor, delivery or in the first few hours after delivery. Sometimes there is enough bleeding to require a blood transfusion.
- Preterm birth. Severe bleeding may prompt an emergency C-section before your baby is full term.
- Placenta accreta Placenta percreta. These are forms of invasive placenta which grow deep into the uterus. The placenta does not detach and deliver as usual. Patients may have severe bleeding which can put the mother's life in danger. This complication usually is usually the result of anterior placenta previa overlying the cesarean scar in women who have had prior cesarean deliveries. The risk for placenta accreta / percreat increases with the number of prior cesarean deliveries.

Shortened/ Dilated Cervix
The cervix is the 'plug' that holds the pregnancy in the uterus. We want it to hold the pregnancy in tight while you walk, run or exercise, but we want it to dilate to 10 cm to allow vaginal birth at term. Considering the weight of the pregnancy, that's a very special plug!!
The closed cervix should measure at least 30 mm at this time- and is often over 40 mm (Caution: a full urinary bladder or focal uterine contraction can elongate the perceived cervical length and make it appear longer than it really is).
A shortened cervix indicates a higher risk for preterm delivery with the highest risk of extreme prematurity for patients with cervical length of less than 20 mm. Read more about prematurity, prevention and treatment.
Cervical shortening and/ or dilatation usually does not occur until after 18 weeks, simply because there isn't enough weight from the pregnancy to test it before then. Any bleeding after 16-18 weeks should be taken seriously because it could indicate cervical shortening or dilatation.
Fetal Issues
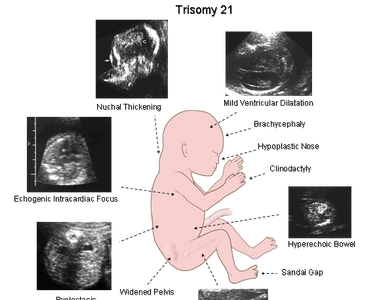
Ultrasound 'Soft Markers'
There are a number of potential nonstructural or minor markers which may be seen at the time of the fetal anatomic scan around 20 weeks. These findings may sometimes indicate an underlying chromosome abnormality, like Down syndrome or other fetal abnormality, but are most often seen as a normal variant. As an isolated finding, these findings usually do not significantly change the risk. They are simply a reminder to take a good look at the baby. Also correlate with your first trimester screen or any other screening you might have had. For extra additional reassurance, you might choose an NIPT test to confirm the chromosomes are normal.
The most common markers include:
- Echogenic intracardiac focus- a bright spot of spots, usually in the left ventricle. Most often seen in normal fetuses (2-3%), and even more common among Asians (up to 10%). Seen in about 30% of fetuses with trisomy 21 (Down syndrome) and 40% of trisomy 13.
- Choroid plexus cysts- fluid spaces within the choroid. The choroid are gland like structures located in the lateral ventricles of the brain, and secretes cerebrospinal fluid. These always go away by 22-24 weeks, even among fetuses with chromosome abnormalities. Seen in 1-2% of normal fetuses, up to 10% of fetuses with Down syndrome and 40% of those with trisomy 18.
- Renal pyelectasis- extra fluid within the collecting system of the kidneys. This is a common normal variant, seen more often in male fetuses compared to females. It occasionally is a sign of fetal Down syndrome but, if not normal, is more likely to indicate an underlying urinary abnormality.
- Single umbilical artery- seen in 1 in normal 200 pregnancies, this is when there is a single umbilical artery rather than the normal paired two arteries. This may be seen in fetuses with trisomy 13 or 18, but those fetuses always show additional abnormalities. There is also a weak association with lower growth in the 3rd trimester for some fetuses.
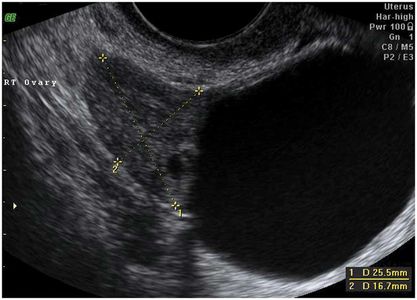
OVARIAN CYST FOUND DURING PREGNANCY
Is it an ovarian cyst? It could be hydrosalpinx, endometrioma, or paraovarian cyst.
OVARIAN CYST DURING PREGNANCY
Every pregnant woman should have an ovarian cyst. This cyst is the corpus luteum, the “cyst of pregnancy,” which produces the hormone Progesterone. All pregnancies are dependent upon progesterone for the first 10-12 weeks of gestation. When the corpus luteum is surgically removed before 11 weeks gestation, most pregnancies will end in miscarriage. Miscarriage can be prevented with progesterone supplementation until 12 weeks gestation.
Most corpus luteum measure less than 5 cm. Sometimes we discover ovarian cysts which are larger than 5 cm, and which persist past 12 weeks. Ovarian cysts in pregnancy can be categorized as follows:
- Size: less than 5 cm, 5-10 cm, greater than 10 cm.
- Description:
- simple: like a water filled balloon
- complex: like a water filled balloon filled with other water filled balloons or dividing lines
- complex with solid components: By far the most common ovarian mass discovered during pregnancy is a dermoid, or dermoid cyst. These have a characteristic appearance but can be easily missed by ultrasound, even when very large because the often look similar to adjacent fat.
The need to worry, or the medical indication to intervene (to remove the cyst with surgery) is based on the combination of size, description, gestational age and symptoms. One end of the spectrum is the Absolute Need to remove a 12 cm cyst that is clearly causing pain at 15 weeks of pregnancy. The other end of the spectrum is warning Against removing a 4 cm simple cyst that is not causing any pain. Most patients have something in between.
Which Cysts to Follow
Ovarian cysts can lead to a number of potential problems. In pregnancy the problems are more acute in the asymptomatic phase because the risk of premature delivery caused by (or associated with) surgical intervention Increases with gestational age after approximately 20 weeks. Also, the window for laparoscopic surgical management of ovarian cysts closes as the pregnancy continues past 20 weeks.
The Potential Problems
- Pain: We can’t predict which cysts will cause, or continue to cause pain. Cysts can cause the ovary to twist on its blood vessels. Torsion (twisting) REALLY HURTS and can damage the ovary; it can only be treated with surgery. A cyst size over 5 cm can be, but is not always, associated with pain.
- Rupture: ALMOST NEVER HAPPENS.
- Cancer: during pregnancy this is a rare but serious finding.
- Size and Surgery: as the cyst gets bigger, assuming it is not cancer, it becomes harder to remove the cyst without removing the entire ovary. It is really important to avoid taking out ovaries in women considering pregnancy in their future.
Third TrimesteR ISSUES

Growth restriction
The third trimester is the true time for incubation and growth. After 24 weeks, babies continue to grow in length at the same rate but now accelerate growth and maturation Your baby is formed, but needs to mature and grow, and get ready for the outside world. The primary issues to watch for are:
- Preterm delivery
- Pre-eclampsia/ hypertension (more common with first time mums)
- Growth delay
- Gestational diabetes
It's important to distinguish SGA (small for gestational age) babies from those with IUGR (intrauterine growth restriction). Most small babies are perfectly healthy. In fact, if we knew that all small babies are healthy, both patients and doctors might be saying the smaller the better (at least in terms of birth itself). Of course we don't say that, but it's to emphasize that size is not the issue; health is the issue (that's true after birth as well!). Most small babies are small because they were meant to be that way- it's programmed into their DNA, usually based on parent size (maternal contribution probably more important than paternal before birth). True IUGR implies that the baby is small because it's not getting enough of what it needs. A mother's diet is almost always sufficient for baby's growth, so that's not the issue. What then? The answer of course lies with the placenta- the mediator between mother and baby. If the placenta is not functioning properly then baby may not grow as is it should. In addition to smaller baby size, other clues to placental dysfunction include
- decreased amniotic fluid
- Abnormal Doppler studies (umbilical, middle cerebral artery)
- Decreased fetal activity (late stages)
This and other potential complications of pregnancy are covered in a separate post.
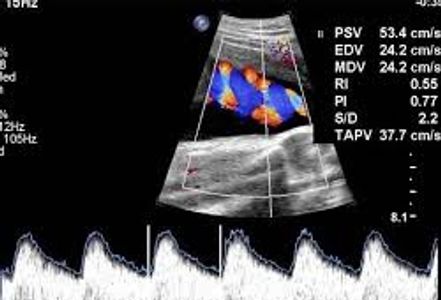
Doppler studies
Doppler studies of the umbilical artery, middle cerebral artery, and the uterine arteries can help confirm that baby is getting sufficient blood delivered to the placenta. Increased resistance of the umbilical artery Doppler can indicate growth restriction, preeclampsia, or elevated blood pressure.
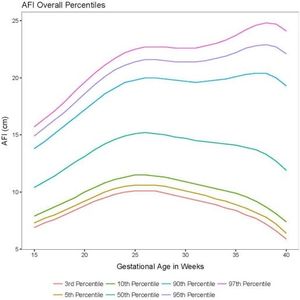
Amniotic Fluid
Amniotic fluid varies widely but in general we would like to see an amniotic fluid index (AFI) of between 8 and 22. Increased fluid most commonly reflects larger fetal size, with or without gestational diabetes. Sometimes increased amniotic fluid (polyhydramnios) in the 3rd trimester can indicate an underlying fetal abnormality, such as a chromosome abnormality, diaphragmatic hernia, or esophageal atresia. An underlying fetal abnormality is especially likely with greater degrees of polyhydramnios, and if the baby is small.
Note in the graph that the lower range for low amniotic fluid starts to decrease after 25 weeks, and can drop off quickly close to term. For this reason, amniotic fluid needs to be watched closely near term. Low amniotic fluid can lead to stillbirth, probably due to compression of the umbilical cord.
Uterine Issues
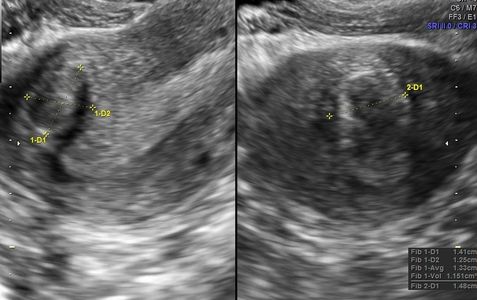
Fibroids
Fibroids appear as discrete structures in the wall of the uterus, although sometimes they grow into the uterine cavity. Fibroids closest to the uterine cavity (endometrium) are most likely to cause symptoms of bleeding. Types of Fibroids
- Intramural fibroids – They develop in the muscle of the womb. If large enough, they can distort the shape of the uterus and cause heavy periods, pain and pressure.
- Subserosal fibroids – they originate in the muscle wall but protrude outside the womb into the pelvis.
- Submucosal fibroids – they grow into the inner cavity of the womb and are more likely to cause bleeding problems or difficulties when trying to conceive.
In almost all cases, the fibroids will shrink and may eventually disappear after menopause.
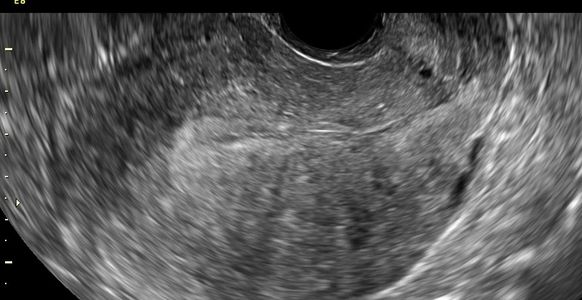
Adenomyosis
Adenomyosis typically presents with an enlarged uterus. The myometrium is thickened and non-uniform (heterogeneous) with a 'streaky' appearance. Fibroids are often absent, but co-existing fibroids are not unusual.

Uterine Congenital Abnormalities (Duplication etc)
Bicornuate uterus appears similar to septated uterus, but the outer fundus no longer has the normal rounded shape. Instead, the outer shape shows a mid indentation at least 1cm and a wide intercornual (tube) distance that can be appreciated via hysteroscopy, as well as laparoscopy. A bicornuate uterus cannot be treated with simple resection and therefore surgery is not indicated. However, there is an increased risk of recurrent pregnancy loss, cervical incompetence, and preterm delivery. Many patients are told they have a bicornuate uterus when, in fact, they may have an arcuate uterus or septated uterus.
Endometrial Issues

Polyps
Endometrial polyps show as focal echogenic areas which obscure the normal central interface. A vascular pedicle, when present, helps to confirm a polyp.
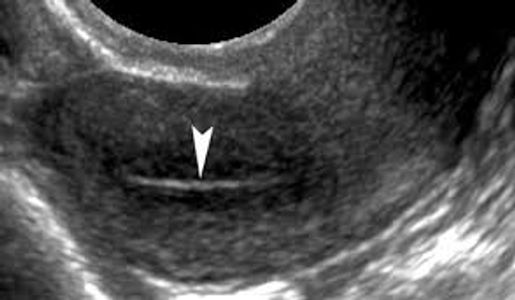
Atrophy
Endometrial atrophy is the most common cause of bleeding among postmenopausal women. This may also occur from hormonal suppression- such as oral contraceptives.

Hyperplasia
Hyperplasia may be seen with excessive unopposed estrogen, tamoxifen and in some patients with polycystic ovarian syndrome. Endometrial hyperplasia is usually caused by an excess of estrogen without progesterone (female hormones). The lining of the uterus is not shed if ovulation does not occur. This means that the endometrium may continue to grow in response to the production of estrogen. The cells of the endometrium may abnormally crowd (hyperplasia), which may lead to the cancer of the uterus.
Atypical endometrial hyperplasia is a premalignant condition of the endometrium. It occurs when there is an overgrowth of abnormal cells, or it may develop from endometrial hyperplasia. In some cases, polyps (tumors) in the uterus can lead to atypical endometrial hyperplasia. It is caused by unopposed estrogen from a number of factors including:
- Hormone changes during menopause (cessation of menstrual period)
- Polycystic ovarian syndrome
- Estrogen-hormone replacement therapy
- Breast cancer treatment, using drugs such as tamoxifen (Nolvadex®, Tamofen®)
Ovarian Issues
Hemorrhagic Cysts
Non Simple Cysts (I call echogenic cysts)
- Functional Cysts
- Hemorrhagic cyst- resolve within 6 weeks
- Paraovarian cyst- rarely hemorrhagic
- Endometriomas
- Tubal (hematosalpinx, pyosalpinx)
- Pseudocyst (loculated peritoneal fluid with adhesions)
- Benign Tumors
- Dermoid cysts - Other benign tumors
- Malignant tumors (Cancer)
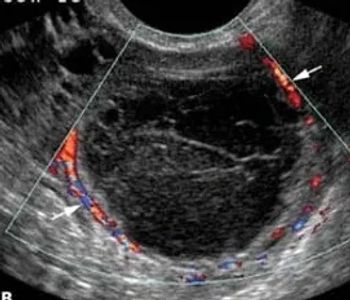
Of these, hemorrhagic cysts, endometriomas, and dermoids are by far the most likely. Hemorrhagic cysts result from rupture of blood vessels, usually at the time of ovulation. They are variable in size and echo pattern. They show no internal vascularity but usually show peripheral vascularity, which can be quite prominent. Hemorrhagic cysts may be very painful and cause women to go to A&E (emergency room)

Endometriomas
Endometriomas are focal collections of blood due to endometriosis. These typical show mid level uniform internal echogenicity due to recurrent hemorrhage. The outer wall is often thickened or partially thickened. They may show punctate calcifications of the outer wall. They show no internal vascularity and little to no peripheral vascularity.
Dermoid
Most ovarian tumors are benign. Among these, the most common is a dermoid, or dermoid cyst. Most dermoids are entirely asymptomatic- women are not aware they have them. They are usually discovered during a pelvic exam or a pelvic ultrasound performed for other reasons. However, some tumors, like dermoids, may be associated with pelvic pain if they cause torsion, or partial torsion of the ovary.
Images of IUD Placement
Normal
Low Position IUD
Low Position IUD

Normal position of an IUD seen on coronal 3D images.
Low Position IUD
Low Position IUD
Low Position IUD
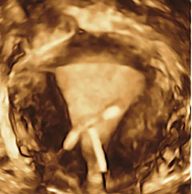
Low and mildly oblique position of an IUD seen on coronal 3D images.
IUD placement
Low Position IUD
IUD placement
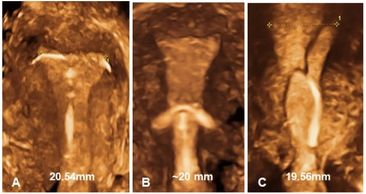
A, normal; b, low position; and c, oblique position of IUDs, seen on coronal 3D images.